| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 颅内肿瘤-转移性恶黑
-
本帖最后由 于 2006-10-09 09:50:00 编辑
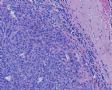
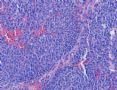
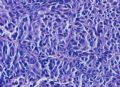
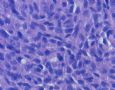
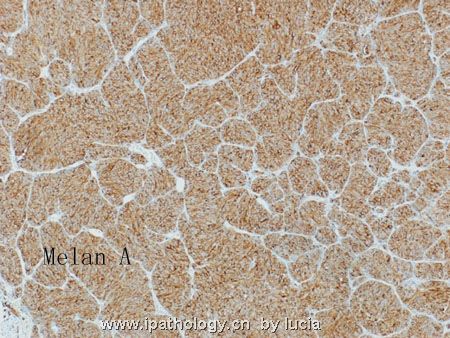
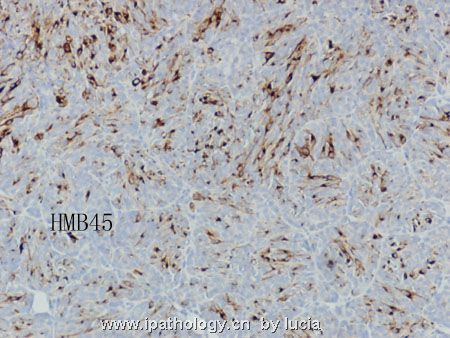
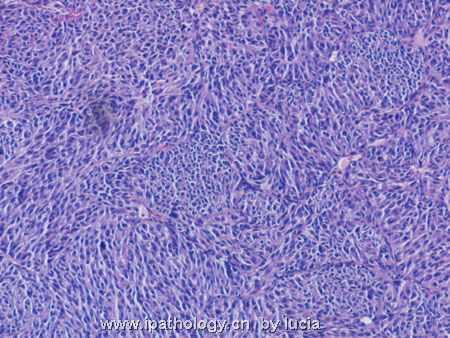
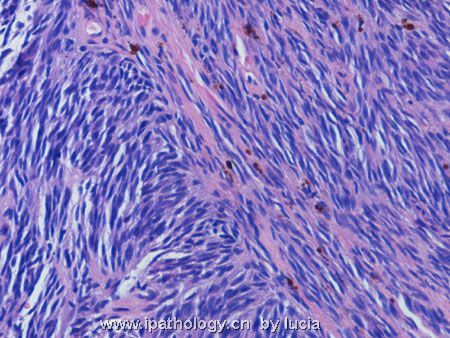
Key features observed are circumscribed tumor border (assuming this is representative of the entire tumor border), high cellularity, focal nesting pattern, oval to slightly elongated nuclei, faintly eosinophilic cytoplasm, and poor differentiation towards epithelial, glial or neuronal lineages. A cerebellar tumor in a 61-yr-old woman with such histopathology and strong S100 immunoreactivity has two directions of diagnostic interpretation - secondary (metastasis) or primary tumor. Clinical implication and further management of the two directions are very different, and pathologists are charged with this important responsibility. If this is a primary brain tumor, possibilities include medulloblastoma (rare, but does occur in older individuals) and small cell variant of glioblastoma. S100 immunoreactivity effectively rules out large B cell lymphoma. The circumscribed tumor border is not that seen in glioblastomas. If this is a case of medulloblastoma, the large cell/anaplastic variant has to be considered. For some reasons, cerebellum is a preferred site of metastasis in older adults. This preference is disproportionate to its relative volume in CNS and so far has not been satisfactorily explained. Two important differential diagnoses exist in this direction - metastatic melanoma and metastatic small cell (or neuroendocrine) carcinoma. The presence of faintly eosinophilic cytoplasm (without melanin pigment) is against the possibility of metastatic small cell (neuroendocrine) carcinoma. It is hard to tell nuclear chromatin pattern from the uploaded photos. Small cell carcinomas usually do not show large prominent nucleoli, whereas melanomas often do, accompanied by occasional intranuclear pseudoinclusions. Strong and diffuse S100 immunoreactivity is probably the diagnostic clincher of this case. This certainly favors metastatic melanoma over the other possibilities discussed. Before doing more immunohistochemical stains (Melan A, HMB45, GFAP, cytokeratin, synaptophysin) to rule in melanoma and to rule out small cell carcinoma and medulloblastoma, I would check the patient's history to see if a known melanoma of skin exists currently or in the past, and whether this is a solitary lesion in CNS (metastasis to brain are often multifocal). If history of melanoma is positive and this is just one of several CNS lesions, the diagnosis of metastatic melanoma is definite. If no such history exists and the lesion appears solitary, I would then proceed with additional stains as listed above to delineate its nature. This case demonstrates a common scenario in our clinical practice - very educational. Thanks.

聞道有先後,術業有專攻
名称:图1
描述:图1
名称:图2
描述:图2
名称:图3
描述:图3
名称:图4
描述:图4
-
Primary melanocytoma (benign; also known as cellular blue nevus or melanotic schwannoma) or diffuse malanosis are very rare conditions of the leptomeninges. Primary melanoma (malignant) of the leptomeninges is even rarer. In fact, it is so rare that each case is worthy of case report in the literature. This diagnosis, of course is one by exclusion of any malignant melanoma in the skin and mucous membrane. On the other hand, metastatic melanoma is quite common in cases of deeply invasive malignant melanoma of skin and, sometimes, mucous membrane. Without a clear knowledge of any past skin disease/surgery history and a thorough survey of the patient's skin and mucous membrane, it is impossible to exclude the possibility of primary melanoma of the leptomeninges in this case. However, with statistics overwhelmingly favoring a metastatic origin, the burden of proof is on those who favor this being a primary melanoma.

聞道有先後,術業有專攻
-
foolishfish 离线
- 帖子:50
- 粉蓝豆:27
- 经验:122
- 注册时间:2007-01-18
- 加关注 | 发消息
-
本帖最后由 于 2007-03-16 20:47:00 编辑
| 以下是引用mjma 在2006-10-9 9:46:00的发言(第4楼): Key features observed are circumscribed tumor border (assuming this is representative of the entire tumor border), high cellularity, focal nesting pattern, oval to slightly elongated nuclei, faintly eosinophilic cytoplasm, and poor differentiation towards epithelial, glial or neuronal lineages. A cerebellar tumor in a 61-yr-old woman with such histopathology and strong S100 immunoreactivity has two directions of diagnostic interpretation - secondary (metastasis) or primary tumor. Clinical implication and further management of the two directions are very different, and pathologists are charged with this important responsibility. If this is a primary brain tumor, possibilities include medulloblastoma (rare, but does occur in older individuals) and small cell variant of glioblastoma. S100 immunoreactivity effectively rules out large B cell lymphoma. The circumscribed tumor border is not that seen in glioblastomas. If this is a case of medulloblastoma, the large cell/anaplastic variant has to be considered. For some reasons, cerebellum is a preferred site of metastasis in older adults. This preference is disproportionate to its relative volume in CNS and so far has not been satisfactorily explained. Two important differential diagnoses exist in this direction - metastatic melanoma and metastatic small cell (or neuroendocrine) carcinoma. The presence of faintly eosinophilic cytoplasm (without melanin pigment) is against the possibility of metastatic small cell (neuroendocrine) carcinoma. It is hard to tell nuclear chromatin pattern from the uploaded photos. Small cell carcinomas usually do not show large prominent nucleoli, whereas melanomas often do, accompanied by occasional intranuclear pseudoinclusions. Strong and diffuse S100 immunoreactivity is probably the diagnostic clincher of this case. This certainly favors metastatic melanoma over the other possibilities discussed. Before doing more immunohistochemical stains (Melan A, HMB45, GFAP, cytokeratin, synaptophysin) to rule in melanoma and to rule out small cell carcinoma and medulloblastoma, I would check the patient's history to see if a known melanoma of skin exists currently or in the past, and whether this is a solitary lesion in CNS (metastasis to brain are often multifocal). If history of melanoma is positive and this is just one of several CNS lesions, the diagnosis of metastatic melanoma is definite. If no such history exists and the lesion appears solitary, I would then proceed with additional stains as listed above to delineate its nature. This case demonstrates a common scenario in our clinical practice - very educational. Thanks. |

- 境随心转
-
本帖最后由 于 2007-03-16 20:48:00 编辑
(第6楼)
非常感谢mjma医师的鉴别诊断。
本例最终诊断是转移性恶黑。
该肿瘤显示了2种不同的形态特征。大部分区域肿瘤细胞卵圆形,排列呈巢状,细胞巢周围包绕纤维血管组织。而其它区域的肿瘤细胞显示梭形的核,束状排列。根据这些特征,应该考虑:1、原发性肿瘤如胶质肉瘤、恶性脑膜瘤;2、转移性肿瘤。整个肿瘤组织内未见任何原纤维背景,胶质肿瘤可以除外。由于肿瘤完全在小脑内生长,所以也不太可能是脑膜起源的肿瘤。如果是转移性肿瘤,那么就应该考虑黑色素瘤(巢状和梭形区域共存)、神经内分泌肿瘤(细胞巢间见纤维血管间隔)以及低分化癌。免疫组化显示肿瘤细胞表达S100、 Melan-A以及HMB45阳性,只是没有观察到黑色素;而CK、Syn 、CgA以及GFAP均示阴性。
患者目前无任何原发肿瘤病史。手术后很快死亡。颅内肿块是单个的。
- 境随心转
-
本帖最后由 于 2007-03-16 20:50:00 编辑
| 以下是引用mjma 在2006-10-21 10:03:00的发言(第11楼): Primary melanocytoma (benign; also known as cellular blue nevus or melanotic schwannoma) or diffuse malanosis are very rare conditions of the leptomeninges. Primary melanoma (malignant) of the leptomeninges is even rarer. In fact, it is so rare that each case is worthy of case report in the literature. This diagnosis, of course is one by exclusion of any malignant melanoma in the skin and mucous membrane. On the other hand, metastatic melanoma is quite common in cases of deeply invasive malignant melanoma of skin and, sometimes, mucous membrane. Without a clear knowledge of any past skin disease/surgery history and a thorough survey of the patient's skin and mucous membrane, it is impossible to exclude the possibility of primary melanoma of the leptomeninges in this case. However, with statistics overwhelmingly favoring a metastatic origin, the burden of proof is on those who favor this being a primary melanoma. |

- 境随心转