| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
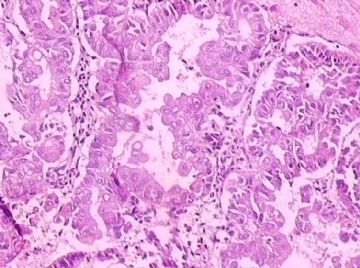
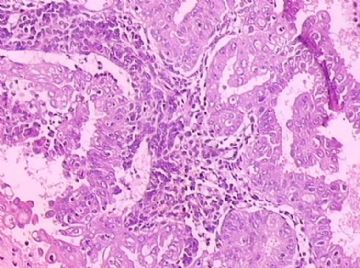
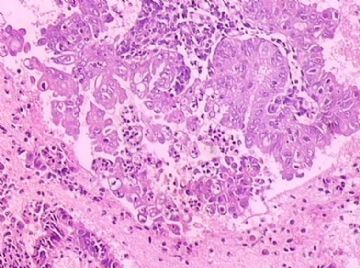
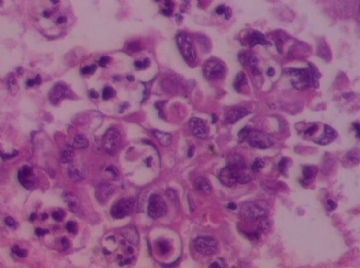
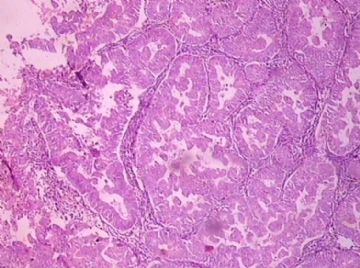
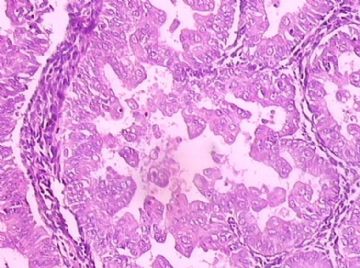
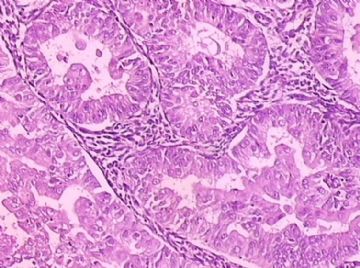
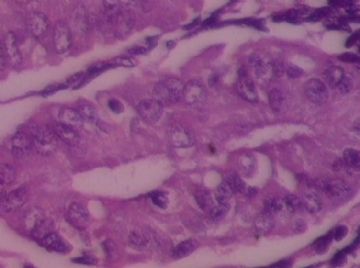
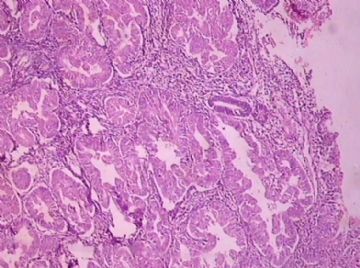
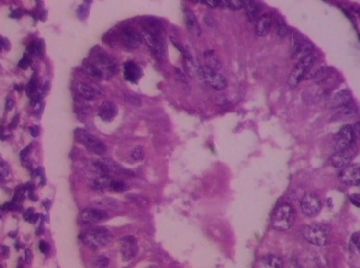
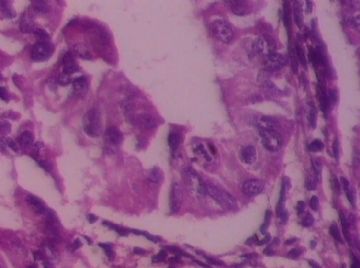
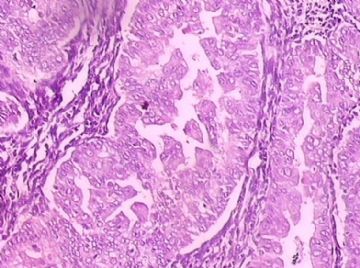
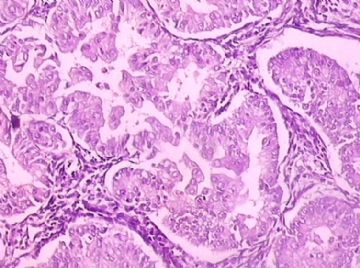
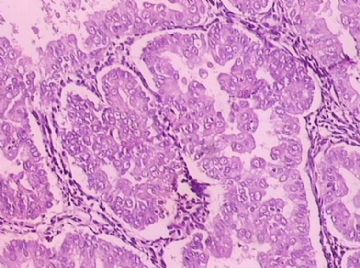
- B172344岁子宫内膜标本,请各位老师会诊,谢谢
| 姓 名: | ××× | 性别: | 女 | 年龄: | 44 |
| 标本名称: | 刮宫标本 | ||||
| 简要病史: | 阴道不规则流血20天 | ||||
| 肉眼检查: | 灰红组织一堆,直径3厘米 | ||||
-
本帖最后由 于 2009-05-14 20:36:00 编辑

- 努力的工作,快乐的生活!
相关帖子
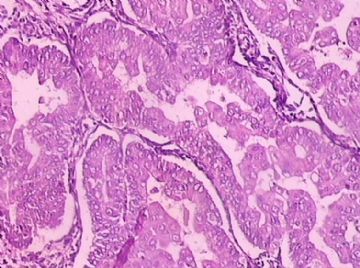
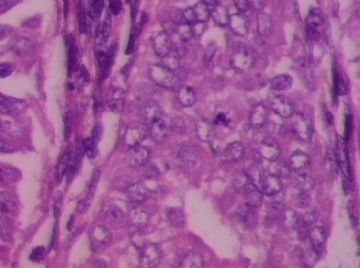
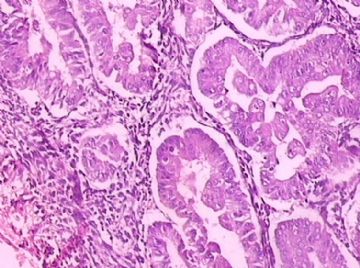
Uterine Endometrioid Carcinoma with Small Nonvillous Papillae: An Analysis of 26 Cases of a Favorable-Prognosis Tumor To Be Distinguished from Serous Carcinoma.
James Homer Wright Pathology Laboratories of the Massachusetts General Hospital and the Department of Pathology, Harvard Medical School.
We have encountered a number of endometrioid carcinomas with small papillary buds lacking fibrovascular cores that could be confused with the small cellular papillae of serous papillary carcinoma (SPC). We have designated these tumors "endometrioid carcinoma with small nonvillous papillae" (ECSP). Because they have not been investigated previously we analyzed 26 examples and compared their features with those of 21 SPCs of the uterus. Three hundred and ninety consecutive cases of endometrial carcinoma diagnosed between January, 1989, and January, 1994, were retrieved from our hospital files; 26 (6.7%) of them, (8% of the endometrioid carcinomas) were identified as ECSP, and 21 (5.4%) as SPC. Tumors were classified as ECSP when the small papillae were present within the glands of otherwise typical endometrioid carcinoma or on the villous projections of villoglandular endometrioid carcinoma. Most of the papillae were in the form of buds of cells with ample eosinophilic cytoplasm and a low nuclear-to-cytoplasmic ratio, but some papillae had a more complex pattern. The papillae arose on a background of International Federation of Gynecology and Obstetrics (FIGO) grade 1 or 2 endometrioid carcinomas, which showed squamous differentiation in half the cases. SPCs were identified according to generally accepted criteria. The mean age of the patients with ECSP was 67 years, intermediate between that of the patients with endometrioid carcinoma lacking small nonvillous papillae (62 years) and that of the patients with SPC (71 years). Patients with ECSP more frequently presented at an earlier stage (73% stage I/II) than those with SPC (29% stage I/II). The overall 5-year survival of patients with ECSP was 84% (95%CI: 0.68-1), more than double that of patients with SPC, 33% (95%CI: 0.10-0.56). ECSP may be confused with SPC on microscopic examination but has clinical and pathological features similar to those of endometrioid carcinoma lacking small nonvillous papillae, and unlike SPC, should be treated in the same manner as the former. Int J Surg Pathol 8(4):279-289, 2000
-
wangdingding 离线
- 帖子:1474
- 粉蓝豆:98
- 经验:6042
- 注册时间:2006-10-19
- 加关注 | 发消息
-
liguoxia71 离线
- 帖子:4174
- 粉蓝豆:3122
- 经验:4677
- 注册时间:2007-04-01
- 加关注 | 发消息