本帖最后由 于 2009-04-30 03:51:00 编辑
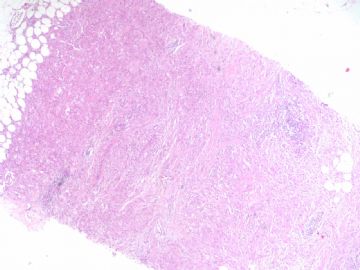
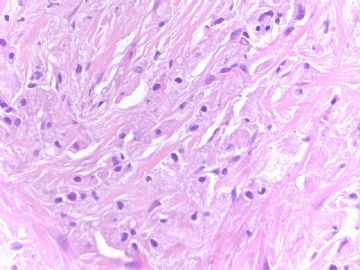
In fact this is a very easy and unusual case which I had when I was at AFIP. I first saw the case. Clearly it was granular cell tumor by cytomorphology. Tumor cells show small round and nuiform nuclei and abundent and granular eosinophilic cytolasm, classic features of GCT. Surprisingly IHC stains indicated the tumor cells were strongly positive for CK7, AE1/AE3, and negative for S-100, CD68. So it is histiocytoid carcinoma, a variant of lobular carcinoma.
Of cause I am sure all of us know that these two tumors have much different prognosis.
The lession for this case is that pathologists must rule out all other possible differential diagoses before we make our final diagnosis in our clinical practice. This priciple should be used for all cases even though we think we know the dx of the cases.
In fact this is a very easy and unusual case which I had when I was at AFIP. I first saw the case. Clearly it was granular cell tumor by cytomorphology. Tumor cells show small round and nuiform nuclei and abundent and granular eosinophilic cytolasm, classic features of GCT. Surprisingly IHC stains indicated the tumor cells were strongly positive for CK7, AE1/AE3, and negative for S-100, CD68. So it is histiocytoid carcinoma, a variant of lobular carcinoma.
Of cause I am sure all of us know that these two tumors have much different prognosis.
The lession for this case is that pathologists must rule out all other possible differential diagoses before we make our final diagnosis in our clinical practice. This priciple should be used for all cases even though we think we know the dx of the cases.