| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
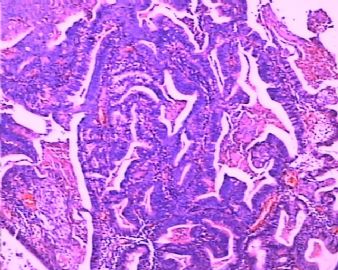
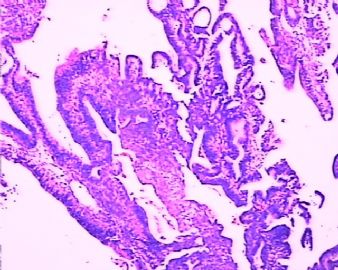
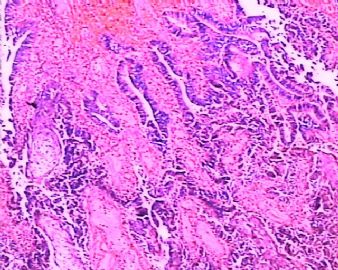
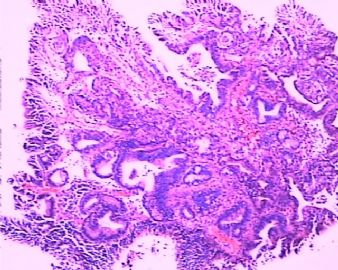
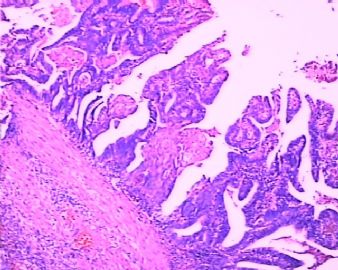
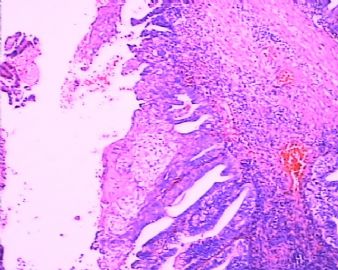
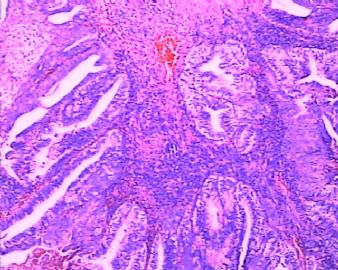
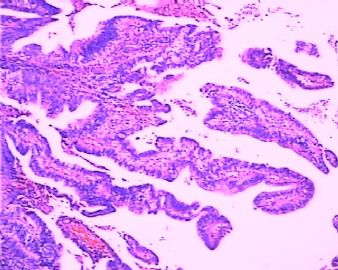
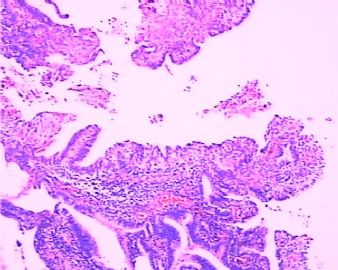
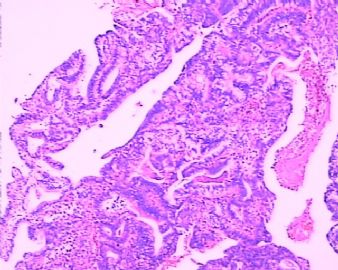
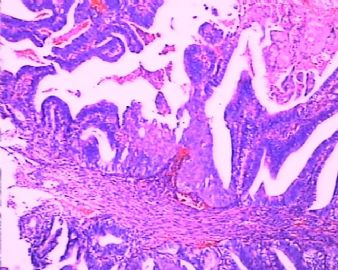
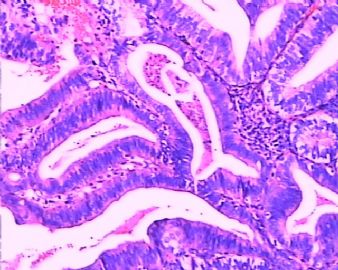
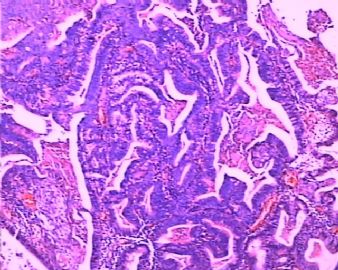
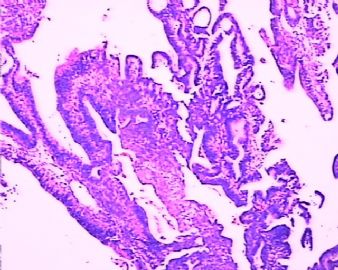
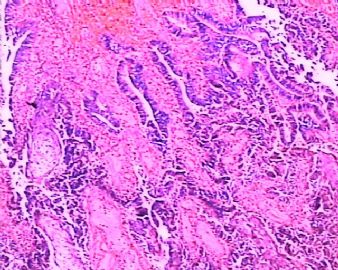
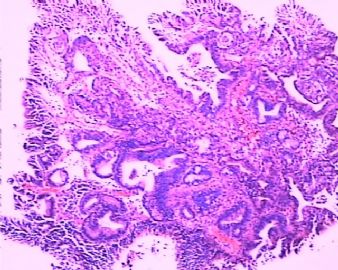
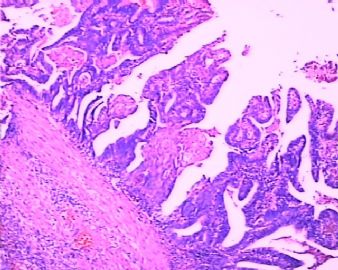
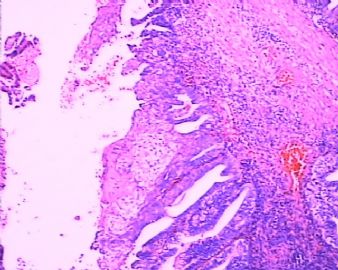
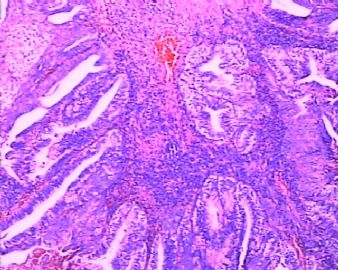
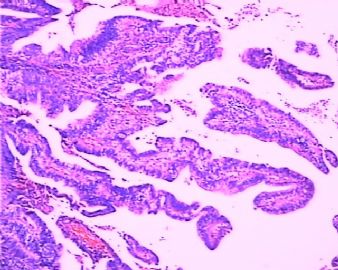
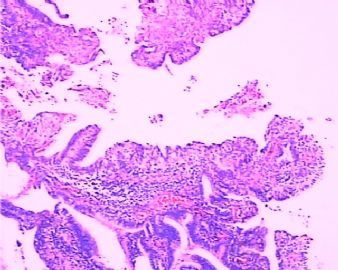
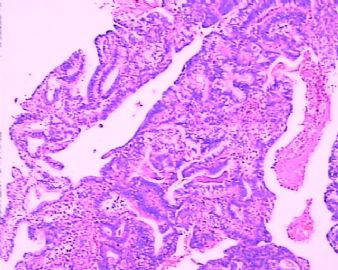
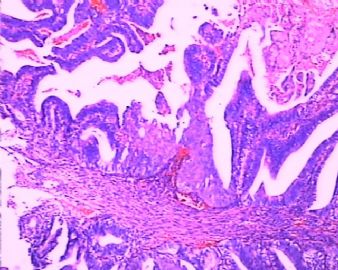
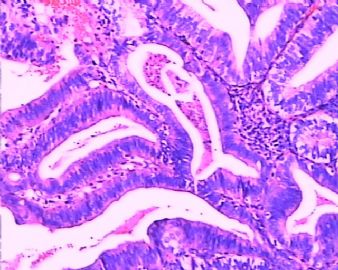
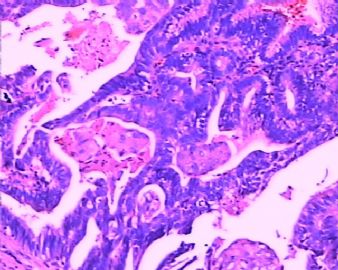
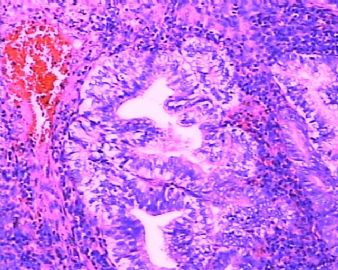
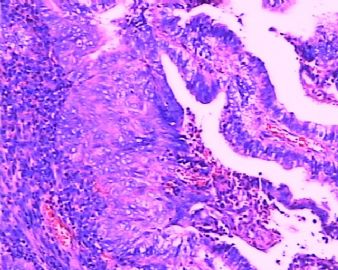
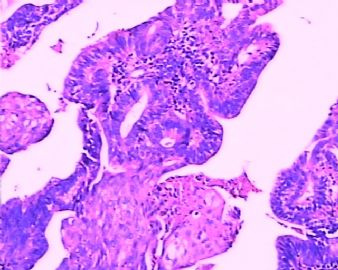
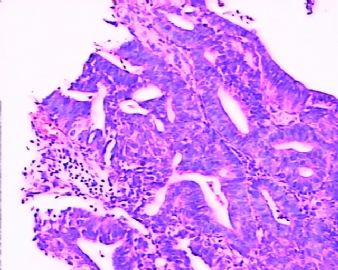
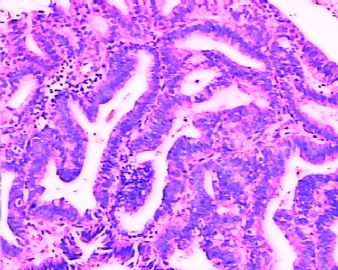
- 腺癌?腺瘤?-宫颈、内膜来源?(临床再次活检,支持子宫内膜来源!!)
-
yoyo751102 离线
- 帖子:303
- 粉蓝豆:72
- 经验:489
- 注册时间:2007-08-20
- 加关注 | 发消息
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
-
本帖最后由 于 2009-04-08 14:32:00 编辑
-
vitamin-xbl 离线
- 帖子:383
- 粉蓝豆:0
- 经验:431
- 注册时间:2007-04-03
- 加关注 | 发消息
good case!
实际上,图片所显示的形态包括宫内膜样腺体结构、绒毛腺管结构等即可见于宫颈,也可见于宫内膜。即便看到癌组织与正常宫颈粘膜的移行也不足以说明它一定是宫颈原发的,如果看不到正常宫颈粘膜,更难判断肿瘤的真正来源了。这种情况只能密切结合临床和影像学(主要是B超)检查。
如果是子宫内膜来源,像息肉一样脱垂至宫颈,而宫颈管粘膜没有受侵犯的话,患者预后可能会较好些,治疗倾向于保守。如果源自子宫内膜而且累及宫颈管,或源自宫颈管,则可能难保生有能力了。

- If you have great talents, industry will improve them; if you have but moderate abilities, industry will supply their deficiency. 如果你很有天赋,勤勉会使其更加完美;如果你能力一般,勤勉会补足其缺陷。
非常感谢杨斌老师的教导!
一个正确的诊断不仅要符合临床,逻辑,形态学,更要具有生物学和分子生物学的支持,那么就能对病人和自己交上一个满意的答卷。
“establishing a logic thought process for differential diagnoses and then leading us to a pathway for rendering correct diagnosis is.”说到这里,我不得不对自己的诊断思路打个大的问号。我也好想像杨老师们一般具有一个正确的思路,以减少漏诊、误诊的机率。可是,自己是处于一个自学的阶段,也不知怎么去做好它。 只有多听听您们的意见,勇于坦诚自己的思想,希望各位老师多多指教为谢!
只有多听听您们的意见,勇于坦诚自己的思想,希望各位老师多多指教为谢!

- 能给人们带来幸福的花儿啊,一定在哪里悄悄地开放
I will be very cautious to make a diagnosis of "endocervical adenocarcinoma" in this case, given her unusual history of amenorrhea for 9 months, abdominal pain and a "cervical mass with 绒毛状 appearance. Also it is very alarming to making an diagnosis of edocervical adenocarcinoma with <5% Ki-67 and p16 negative too.
This case reminds me of a case sending us for consultation a while ago from other hospital. It was a relatively young woman at her 40th with a mass protruding from cervical os. It was diagnosed as "endometrioid adenocarcinoma" of either endocervical or endometrial origin. Immunostain did not support either endometrial or endocervical origin like this case with a very low Ki-67 labeling. It turns out was a "Prolapsed fallopian tube protruding from the cervical os". The point I try to make here is not provide you a definitive diagnosis of this case, but promote further clinicopathologic correlation for any cases not following the logic process. I would like to attain more clinical presentation of this case before I jump on a diagnosis of "adenocarcinoma".
Also I would like to know what is exact staining pattern of p16. Is any focal or patch staining at all or is it totally negative? Some of the photos look like very tubal metaplastic appearance with possible cilia. Immunostain should show a so-called "mosiac pattern" in tubal metaplasia in endometrium or endocervix, but can be very focal stain or totally negative in normal follopian tube. It should be diffusely positive in endocervical adenocarcinoma or serous adenocarcinoma of the endometrium and the ovary. Of course, you cannot make final diagnosis solely based on p16 stain. But it may provide some clues for further evaluation.
I hope this will stimulate further discussion on this case. Remember, providing a definitive diagnosis is not the goal of this section; establishing a logic thought process for differential diagnoses and then leading us to a pathway for rendering correct diagnosis is.

- 不坠青云之志,长怀赤子之心