| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 左颞部肿瘤
-
zhongshihua 离线
- 帖子:1608
- 粉蓝豆:0
- 经验:1651
- 注册时间:2006-09-11
- 加关注 | 发消息
-
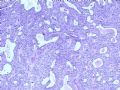
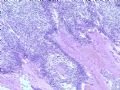
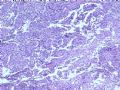
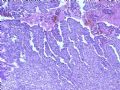
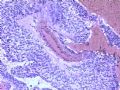
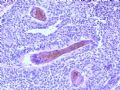
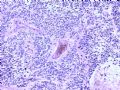
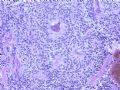
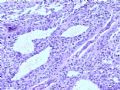
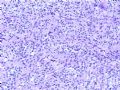
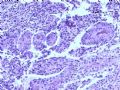
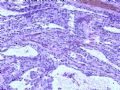
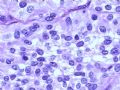
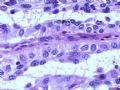
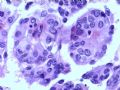
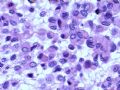
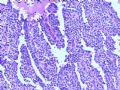
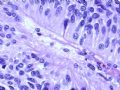
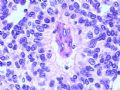
This interesting case is probably a WHO grade III papillary meningioma. It is considered a malignant variant of meningiomas, and can invade local structures, recur, seed through CSF, or even metastasize to extracranial sites. The young patient's age, prominent papillary architecture (perivascular pseudorosettes), relatively uniform cytology, associated necrosis, and local bone invasion are all very characteristic. Some of the discohesive cells even appear "rhabdoid". Mitoses should not be difficult to find, and there usually is no formation of meningothelial whorls or psammoma bodies. Important differential diagnoses include ependymoma and astroblastoma, both could occur in the cerebral surface of young patients. The lack of hyalinized fibrovascular cores is not supportive of astroblastoma. Immunohistochemistry (GFAP, EMA, PR) and reticulin silver stain should be performed to confirm the diagnosis. It is important to know that some meningiomas may have focal GFAP immunoreactivity, but astroblastoma and ependymoma should both have diffuse and strong GFAP immunoreactivity. Some meningiomas are positive for PR, whereas no astroblastoma or ependymoma should express PR. EMA immunoreactivity of ependymoma is characteristically dot-like in the paranuclear region, and patchy and membranous in meningiomas. Reticulin silver stain can highlight slender argyrophilic fibrils radiating from central vessels of papillae.

聞道有先後,術業有專攻
-
zhongshihua 离线
- 帖子:1608
- 粉蓝豆:0
- 经验:1651
- 注册时间:2006-09-11
- 加关注 | 发消息
-
为了学习我翻译了马老师的帖子,不对之处请批评:本例非常有趣,可能是WHO分类的III级乳突状脑膜瘤,被认为是恶性脑膜瘤的一种,可以侵及局部组织,可以复发,也可以经脑脊液种植,甚至转移到颅外部位,患者发病时年龄较青,肿瘤出现明显的乳突状结构(在血管周围形成假的菊形团),细胞大小比较一致,伴有坏死,侵及局部骨是其特征,有时细胞散在似横纹肌样瘤改变。核分裂少见,常常见不到脑膜上皮轮样结构和砂粒体。重要的鉴别诊断包括:室管膜瘤和星形母细胞瘤,这两种肿瘤都可见于年青患者的脑表面。缺乏透明的纤维血管轴心不支持星母细胞瘤。免疫组化和网染可以证实诊断(GFAP, EMA, PR) ,重要的是要了解某些脑膜瘤有局部的GFAP阳性, 但是星母和室管膜瘤的阳性是弥漫和强阳性。有些脑膜瘤PR是阳性,但是星母和室管膜瘤 不表达。室管膜瘤的EMA是特征性的,位于核旁呈点样分布,而脑膜瘤则成斑样、膜样分布。脑膜瘤的网染,非常明显的长梭形的嗜银纤维沿着乳突的血管呈放射状排列。
-
zhongshihua 离线
- 帖子:1608
- 粉蓝豆:0
- 经验:1651
- 注册时间:2006-09-11
- 加关注 | 发消息