| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 遇到成团细胞该怎么办?
-
本帖最后由 于 2009-01-08 19:19:00 编辑
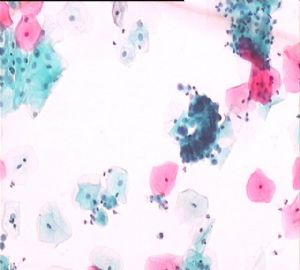
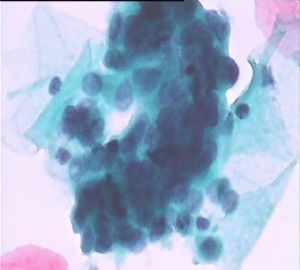
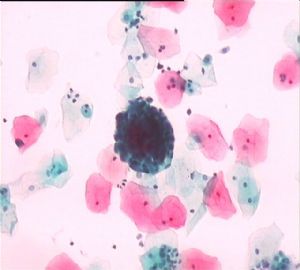
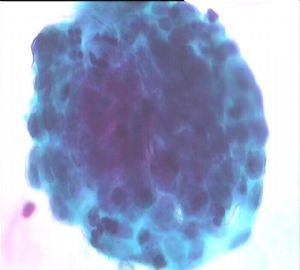
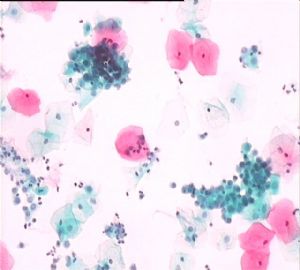
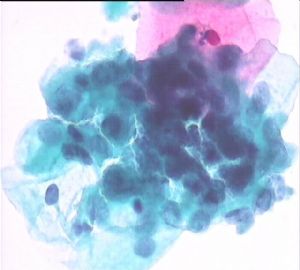
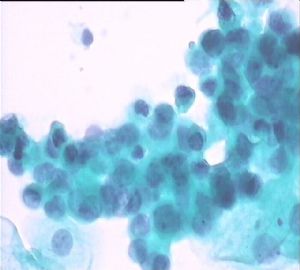
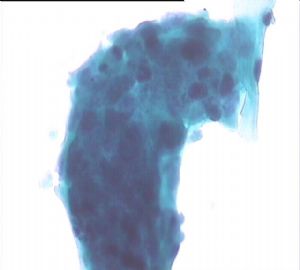
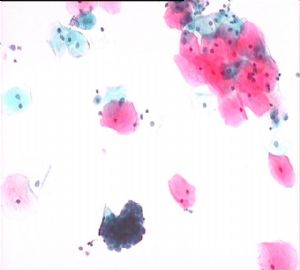
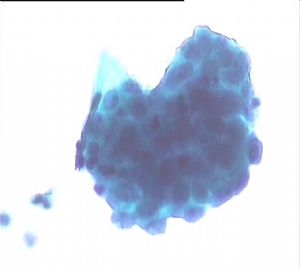
Some clusters are classic exodus endometrial glandular cells surrounding darker staining central aggregates of stromal cells, which can be present in days 6-10. In your case you do not need to mention the em-cells for this age in your report. We will mention normal em-cells only for women 40 or above. Also this women is within day 12.
-
本帖最后由 于 2009-01-08 20:22:00 编辑
赵老师,早上好!(您那当地时间),真的感谢,您这么早就来帮我解决问题。
其实这个病例我个人认为:
1、细胞成团,3D立体结构明显;细胞异形性不明显,来源于宫内膜。
2、尤其地3图和4图应该就是“基质球”,外边是内膜腺细胞,中间是间质细胞。
3、对内膜细胞的不熟悉,和最近这段时间看腺细胞异常的帖子看多了,有点紧张。
4、再是发这个帖子想得到老师们的指点。
5、这个病人是我们本院的医生,找她了解了一些情况,没有感觉到异常和特殊的临床情况;最后我给发了一个NILM,建议定期复查(一年);因为我们这边正常的报告都是这样发的。
哈哈,再次谢谢赵老师,也希望各位老师参与讨论,谢谢!
谢谢以上三位老师的意见,正好这个病例请教一下几位老师的问题是:
1、40岁以下的女性子宫内膜腺癌风险低,在涂片中看子宫内膜细胞不用提及;但是如果看到异常的腺细胞不管多大年龄都得报出,那么也是说其实子宫内膜腺癌还是会发生在40岁以下的妇女对吗?有没有这方面的数据资料呢?
2、子宫内膜腺癌和子宫颈内膜样腺癌的组织学起源是一样的吗?好像不管细胞学还是组织学HE切片判读来源都是很困难的,请问老师有没有这方面比较好的经验和建议呢?
3、现在我了解的资料是HPV-16型主要跟鳞状上皮病变相关,而HPV-18型与腺上皮病变相关;那为什么现在腺上皮的病变不建议做HPV检测呢?
4、现在国内做的HPV检测的方法常用的是HC-2和PCR的方法(听说这个质量控制是一个比较大问题);另听说一些专家说在国外的专家就用液基保存液体同事进行常规细胞学检测和HPV检测,能具体的说说是怎么做的吗?
不好意思,也许我以上的几个问题会占用你们大量的时间,但是我很希望知道这些知识,谢谢!
| 以下是引用兰青风采在2009-1-9 10:44:00的发言:
谢谢以上三位老师的意见,正好这个病例请教一下几位老师的问题是: 1、40岁以下的女性子宫内膜腺癌风险低,在涂片中看子宫内膜细胞不用提及;但是如果看到异常的腺细胞不管多大年龄都得报出,那么也是说其实子宫内膜腺癌还是会发生在40岁以下的妇女对吗?有没有这方面的数据资料呢? 2、子宫内膜腺癌和子宫颈内膜样腺癌的组织学起源是一样的吗?好像不管细胞学还是组织学HE切片判读来源都是很困难的,请问老师有没有这方面比较好的经验和建议呢? 3、现在我了解的资料是HPV-16型主要跟鳞状上皮病变相关,而HPV-18型与腺上皮病变相关;那为什么现在腺上皮的病变不建议做HPV检测呢? 4、现在国内做的HPV检测的方法常用的是HC-2和PCR的方法(听说这个质量控制是一个比较大问题);另听说一些专家说在国外的专家就用液基保存液体同事进行常规细胞学检测和HPV检测,能具体的说说是怎么做的吗? 不好意思,也许我以上的几个问题会占用你们大量的时间,但是我很希望知道这些知识,谢谢! 学习! |

- 学习,学习,再学习!
Briefly answer:
1. of cause, endometrial ca can occur in women younger than 40. Clinically it is not uncommon to meet these kinds of caess. I will let you know if I find a %.
2. About 10-20% endocervical carcinoma are endometrioid types. So you cannot tell the difference by morphology. IHC may be helpful, but a lot of time IHC cannot help. Follow my case of cervical bx with some IHC. I will have some brief introduction.
3. Endocervical ca is related to infection of HPV18, 16 and other types.
ASCCP guidline for AGC, all subcategories (except atypical endometrial cells)
Calposcopy (with endocervical sampling) and
High risk HPV testing (HC-2) and
endometrial sampling (if>35yrs or at risk for endometrial neoplasia)
Endometrial carcinomas are no relation to HPV infection. If you fell comfortable that a case is AGC, endometrial type. Women should have endometrial and endocervical sampling, but no hpv testing.
My study indicated that about 24% women with AGC Pap had positivity for HR HPV test. Literatures review showed the HR HPV positive rate ranges from 20-30% in AGC women. HPV testing can increase the positive predict value of Pap agc. I will let you know if my paper is published. If you are truely interested in AGC, pl check online teaching, my powerpoint talk: a challenge for diagnosis: AGC, ASC-H (081101). I spent a lot of time and review most important related papers for this talk in a conference in the US.
4. This is very complicated topic. It is debatable in the US. Generally speaking HR HPV testing is performed for all ascus women based on the guidline. Others include HPV testing for women>30 years, HPV testing regardless the age depending on clinicians' order. No persons know what will happen in the future.
Hope pathologists can learn the Guideline systemically.
同意赵医生。谢!加几点:
Poin 2: Pathogenesis for endometrial adenocarcinoma includes 2 types: one type related to prolonged estrogen exposure (endometrioid type), another type related to gene mutation (p53, papillary serous type and clear cell type). Pathogenesis for endocervical adenocarcinoma endometrioid type is HPV infection.
Point 3: The worse outcome of atypical endocervical glandular cells is adenocarcinoma in situ (AIS)and invasive adenocarcinoma. Even in these cases, the positive rate for high risk HPV is about 80% (acording to my memory), while the positive rate for squamous cell carcinoma of cervix is >97%. If we rely on HPV test to guide the management of AGC, a significant percentage of AIS and Adeno will be missed. Probably that is why the guideline for AGC is colposcopy. We receive >1000 pap smears a day and we strictly follow guidelines, because if we don't (for example do HPV test for AGC), some insurance may not reimburse us.
Point 4: Yes, we split liquid base pap smear vials for high risk HPV test by HC II and cytology. What we do with the pap smear vials is dictated by clinicians' order with the following categories: regardless HPV test, it means the vials will be divided at accession into 2 portions: one for cytology, one for HPV; reflex HPV, it means when pathologists call the pap ASCUS, the vials will be sent for HPV; HPV for any abnormal cytology, it means normal cytology will not test for HPV, any abnormal cytology such as ASC, LSIL, HSIL, AGC etc will send the vials for HPV. Nowaday, some clinicians request HPV tests only with the liquid base vials without cytology.
Hope it helps.