| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B443(转贴)左踝部肿块--伴有病毒细胞或R-S细胞样细胞的炎性粘液样肿瘤
This uncommon, low grade sarcoma was first described by Montgomery, Devaney, Giordano and Weiss as recently as April, 1998 when they reported 51 cases collected from Sharon Weiss’ consultation files. They named the tumor descriptively, but verbosely, “inflammatory myxohyaline tumor of distal extremities with virocyte or Reed-Sternberg-like cells.” Four month later, the Kindbloms, working in Sweden, reported 44 cases of an identical tumor collected from The Armed Forces Institute of Pathology In Washington, DC and the Sahlgrenska University Hospital in Gothenburg, Sweden. They named it acral myxoinflammatory fibroblastic sarcoma. The sex incidence was equal; the age at diagnosis ranged from 20 to 91, with a median in the fifth decade; tumors were painless and had a long history (median 1 year); were located subcutaneously in the hands, wrists ,feet , and measured from 1 to
Other workers have confirmed the overall accuracy of the original observations with the additional observations that this tumor can occur outside the acral regions on the forearm, arm and thigh and may also behave in a high grade fashion with recurrences and metastases as early as 3 months after the first excision. Before the entity was described, cases were probably diagnosed as peculiar inflammations or low grade myxoid malignant fibrous histiocytomas. The entity is probably much commoner than one would expect with such a recently described tumor.
Prognosis:Combining the two series, 30 of 63 patients with follow up (Recurrences: 48%) experienced one or more recurrences over periods as long as 10 years and two tumors (Metastasis: 3%) metastasized but there were no deaths caused by tumor.
Treatment:Treatment included surgery, radiotherapy and chemotherapy.
-
( 肢端) 黏液炎性纤维母细胞肉瘤( acral myxoinflammatory fibroblastic sarcoma)
是一种好发于肢端的纤维母细胞性肉瘤,含有黏液样区域和炎性纤维性区域,并可见散在性分布的异型大细胞,形态上类似节细胞、R-S 细胞、病毒样巨细胞或多空泡状脂肪母细胞样细胞。由Meis\Kindblom 等于1998 年首先报道,Montgomery 等于同年描述了一组相似的病变,命名为伴有病毒样细胞或R-S细胞样细胞的肢端炎性黏液透明样肿瘤(inflammatory myxohyaline tumor of distal extremities with virocyte or Reed/Sternberg-like cells) ,两者实际上是同一病种采用了不同的名称而已。
临床特点:多发生于40~50 岁间的成年人,年龄范围为4~91 岁,男女均可发病。好发于肢体的远端,约2/ 3 的病例发生于手、腕和前臂远端,1/ 3 的病例发生于足、踝和小腿远端,极少累及肘部和膝部,少数病例发生于躯干和头颈部。临床上表现为局部缓慢生长的无痛性肿块,部分患者曾有外伤史。临床上常被诊断为腱鞘囊肿、腱鞘滑膜炎和腱鞘巨细胞瘤,作者诊断的1 例起先在市疑难病理读片会上,大多数专家均倾向为结节性筋膜炎,但术后不久肿块很快复发,体积巨大,不仅累及足和踝,还延伸至小腿远端,最后患者被做了截肢术 。
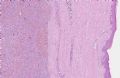
大体表现:界限不清,灰白色,多结节状,直径1~8 cm, 平均314 cm 。
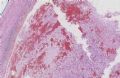
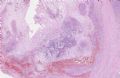
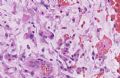
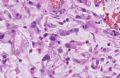
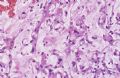
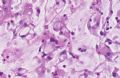
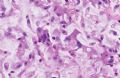
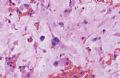
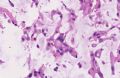
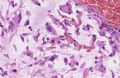
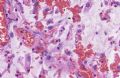
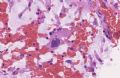
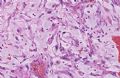
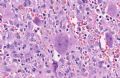
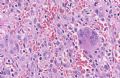
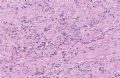
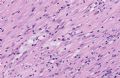
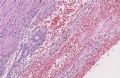
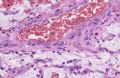
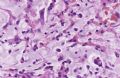
镜下表现:病变呈多结节性,境界不清,常累及关节和腱鞘的滑膜,并浸润至皮下脂肪组织及皮肤的真皮层。低倍镜下显示,病变由黏液样区域、透明变性区域和炎症性区域混合组成 。在大多数病例内,炎症细胞多为淋巴细胞和浆细胞,部分肿瘤内也可见到中性粒细胞和嗜酸性粒细胞,有时可见生发中心形成,炎症性区域内常伴有程度不等的纤维化。黏液样区域和透明变性区域所占的比例因病例而异,有些完全由黏液样区域组成,而另一些肿瘤内,黏液样区域仅为局灶性,两区之间常可见移行。黏液样区域内有时可见黏液湖形成,其内的细胞及血管均较稀疏,可见多空泡状的假脂肪母细胞 。透明样区域由散在的炎症细胞和梭形瘤细胞混合组成,间质呈透明样变性,灶性区域可见含铁血黄素性沉着。在细胞偏丰富的透明样区域内还可见
一些形态不典型的细胞,呈胖梭形、组织细胞样或上皮细胞样。梭形细胞的核具有中等程度的异型性,上皮样或组织细胞样的异型细胞体积较大,核呈空泡状,内含大核仁,胞质呈
嗜酸性,形态上类似R2S 细胞、病毒样细胞(virocyte-like cell) 或节细胞。
免疫组织化学:瘤细胞表达波形蛋白,部分表达CD68 、CD34 和α2SMA , 淋巴细胞多为T 细胞,少数为B 细胞。
超微结构:畸形细胞具有变异纤维母细胞的形态特征。
细胞遗传学: 显示t (1;10) (p22;q24) 易位伴3 号和13 号染色体缺失。免疫荧光原位杂交发现断裂点分别位于1p22 与10q24 的BCL10 基因近端与GO T1 基因远端 。此种罕见的染色体核型改变至今未在其他软组织肿瘤中发现,因而支持该瘤是一种独立的纤维母细胞肿瘤。
鉴别诊断: (1) 腱鞘滑膜炎:主要为炎症性的增生性病变,无异型细胞。(2) 炎性肌纤维母细胞瘤:多见于儿童和青少年,主要发生于肺和腹腔,极少发生于手、足或踝等肢体末端部位。(3) 黏液纤维肉瘤:多发生于肢体的近端,而手足部位很少发生。镜下一般见不到混杂的炎性区域及硬化性区域,也不见类似R2S 或病毒样细胞的畸形大细胞。(4) 霍奇金淋巴瘤:肢端黏液炎性纤维母细胞肉瘤中异型的R2S 样细胞CD15 和CD30 标记均为阴性。
生物学行为:局部复发率为20 %~70 %, 在多次复发的病例中,超过1/ 3 的患者做了截肢术。到目前为止,仅有1 例发生远处转移。