| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
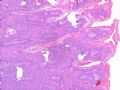
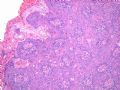
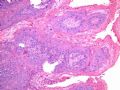
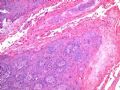
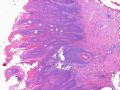
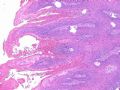
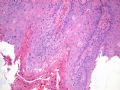
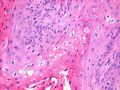
- B516外阴赘生物
| 姓 名: | ××× | 性别: | 年龄: | 82 | |
| 标本名称: | 外阴 | ||||
| 简要病史: | 发现 赘生物3个月 | ||||
| 肉眼检查: | |||||
-
本帖最后由 于 2007-08-17 15:54:00 编辑
相关帖子
- • GYN Case 3 from USCAP 2007
- • 外阴肿物
- • 外阴疣状物
- • 外阴肿块
- • 外阴肿块
- • 欣赏-外阴病变
- • 外阴结节
- • 搞笑病例2__妇科专家不知道外阴派杰病?
- • 外阴粘液性肿物
- • 外阴大肿块
-
Sorry for missing Professor Zhou's teaching on this case and I have no idea what the final diagnosis of Dr. Zhou provides. My two penny personal opinion is a "Warty type of squamous carcinoma" in this 82 year old lady. I do not think this is a verrucous carcinoma due to less impressive "bulky and pushing base" which is vanishingly rare. Also it is way beyond of condyloma cytologically. You have to think three times before to make a diagnosis of condyloma in a 82 year old lady socioeconomically. I am humblely listening to Professor Zhou's comment and critiques here. Thanks you.

- 不坠青云之志,长怀赤子之心
| 以下是引用shihuaiy 在2007-1-30 22:33:00的发言:
外阴疣状肿瘤以湿疣状癌(condylomatous carcinoma)相对较多,疣状癌(verrucous carcinoma)次之,巨大或增生性尖锐湿疣外阴少见。湿疣状癌和疣状癌的区别在于后者异型性较小,HPV以6型多见,乳头中间质不明显。此例有异型性和较多的核分裂像,乳头间质明显,有挖空样细胞,考虑为湿疣样癌(HPV16多见)可能性较大。文献报道该肿瘤预后很好,可以复发但转移少见。等待学习! |
Guide for signing out VIN cases according to new ISSVD Classification:
|
Histology |
Final Diagnosis |
Comment |
|
VIN-1 |
SQUAMOUS EPITHELIUM WITH ATYPIA, CONSISTENT WITH HPV-RELATED CHANGES |
The above lesion is equivalent to vulvar intra-epithelial neoplasia 1(VIN-1) lesion according to the old classification scheme. The new International Society for the Study of Vulvovaginal Disease (ISSVD) classification no longer includes “VIN-1” as a type of VIN. This is due to lack of evidence that “VIN-1” is a cancer precursor lesion. References: J Low Genit Tract Dis. 2007;11:46-47. J Reprod Med. 2005;50:807-10. |
|
VIN-2 or VIN-3 |
VULVAR INTRAEPITHELIAL NEOPLASIA (VIN), USUAL WARTY TYPE.
VULVAR INTRAEPITHELIAL NEOPLASIA (VIN), USUAL BASALOID TYPE.
VULVAR INTRAEPITHELIAL NEOPLASIA (VIN), USUAL MIXED (WARTY/BASALOID) TYPE. |
The above diagnosis is based on the new International Society for the Study of Vulvovaginal Disease (ISSVD) classification of vulvar intra-epithelial neoplasia (VIN). The above lesion is equivalent to VIN-2 (or VIN-3) according to the old classification scheme. Reference: J Low Genit Tract Dis. 2007;11:46-47. |
|
VIN-differentiated type |
VULVAR INTRAEPITHELIAL NEOPLASIA (VIN), DIFFERENTIATED TYPE. |
The above diagnosis is based on the new International Society for the Study of Vulvovaginal Disease (ISSVD) classification of vulvar intra-epithelial neoplasia (VIN). The risk of progression to invasion seems greater in differentiated VIN than in usual VIN. References: J Low Genit Tract Dis. 2007;11:46-47. Int J Gynecol Pathol. 2001;20:16-30. |
-
本帖最后由 于 2009-06-11 05:23:00 编辑
Above is new classification. Condyloma is type of VIN 1. Now diagnosis of VIN1:
SQUAMOUS EPITHELIUM WITH ATYPIA, CONSISTENT WITH HPV-RELATED CHANGES
HPV infection rate is 77% for VIN1 with only 14% HPV 16/18.
HPV infection rate is 77% for VIN1 with only 14% HPV 16/18.
Do we know HPV type for this 82 year-old lady?
-
Obstet Gynecol. 2009 Apr;113(4):917-24.
-
Human papillomavirus type-distribution in vulvar and vaginal cancers and their associated precursors.
Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina, Chapel Hill, North Carolina 27599-7435, USA. jennifers@unc.edu
OBJECTIVE: Data on human papillomavirus (HPV) prevalence in vulvar and vaginal cancers are limited. These data are important to predict the potential future effect of prophylactic HPV vaccines. Our aim was to conduct a systematic review of HPV type distribution in vulvar and vaginal invasive carcinomas, vulvar intraepithelial neoplasia (VIN), and vaginal intraepithelial neoplasia. DATA SOURCES: A MEDLINE search was conducted using the terms vulvar/vaginal cancer, intraepithelial neoplasia, and HPV/human papillomavirus through September 2007 with no specified start date or language restrictions. METHODS OF STUDY SELECTION: A total of 725 abstracts (564 vulvar, 161 vaginal) were reviewed, of which 67 studies (56 vulvar, 11 vaginal) met the inclusion criteria of using polymerase chain reaction (PCR) or hybrid capture assays for HPV DNA detection and having more than one case with HPV data available. TABULATION, INTEGRATION AND RESULTS: This review identified 2,790 vulvar (1,379 invasive, 1,340 VIN2/3, 71 VIN1) and 315 vaginal cases (83 invasive, 166 vaginal intraepithelial neoplasia 2/3, 66 vaginal intraepithelial neoplasia 1). Most cases were from North America and Europe (87.2%), with few from Asia (5.5%) and South America (7.3%). Human papillomavirus prevalence in vulvar cancer, VIN2/3, and VIN1 was 40.1%, 80.4%, and 77.5%, respectively. HPV prevalence in vaginal cancer, vaginal intraepithelial neoplasia (VAIN)2/3, and VAIN1 was relatively higher at 65.5%, 92.6%, and 98.5%, respectively. HPV16 was the most common type in vulvar (29.3%) and vaginal (55.4%) cancers, VIN2/3 (71.2%) and VAIN2/3 (65.8%). CONCLUSION: Human papillomavirus prevalence was higher among vaginal than vulvar cases, and HPV16 accounted for most HPV-positive cases for both cancers. Although the potential effect of HPV vaccines on these gynecologic cancers may not be as high as for cervical cancer due to their more diverse causes, vaccinating young women against HPV16/18 may help to reduce the incidence of HPV-related cases.
-
benben520sps 离线
- 帖子:1045
- 粉蓝豆:568
- 经验:1254
- 注册时间:2009-07-28
- 加关注 | 发消息
-
liziqiang88 离线
- 帖子:957
- 粉蓝豆:262
- 经验:3935
- 注册时间:2007-03-15
- 加关注 | 发消息