| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 微信病例120 | 左乳肿物切除并前哨淋巴结活检。整个肿物大小11mm,一枚前哨淋巴结未检出癌。……,请您参与讨论分析。
-
流光飞舞_nON6327 离线
- 帖子:8
- 粉蓝豆:0
- 经验:8
- 注册时间:2017-05-29
- 加关注 | 发消息
微信群:中美加乳腺病理交流群

孔祥田(Max)*Sacramento*CA] 05-30 04:13
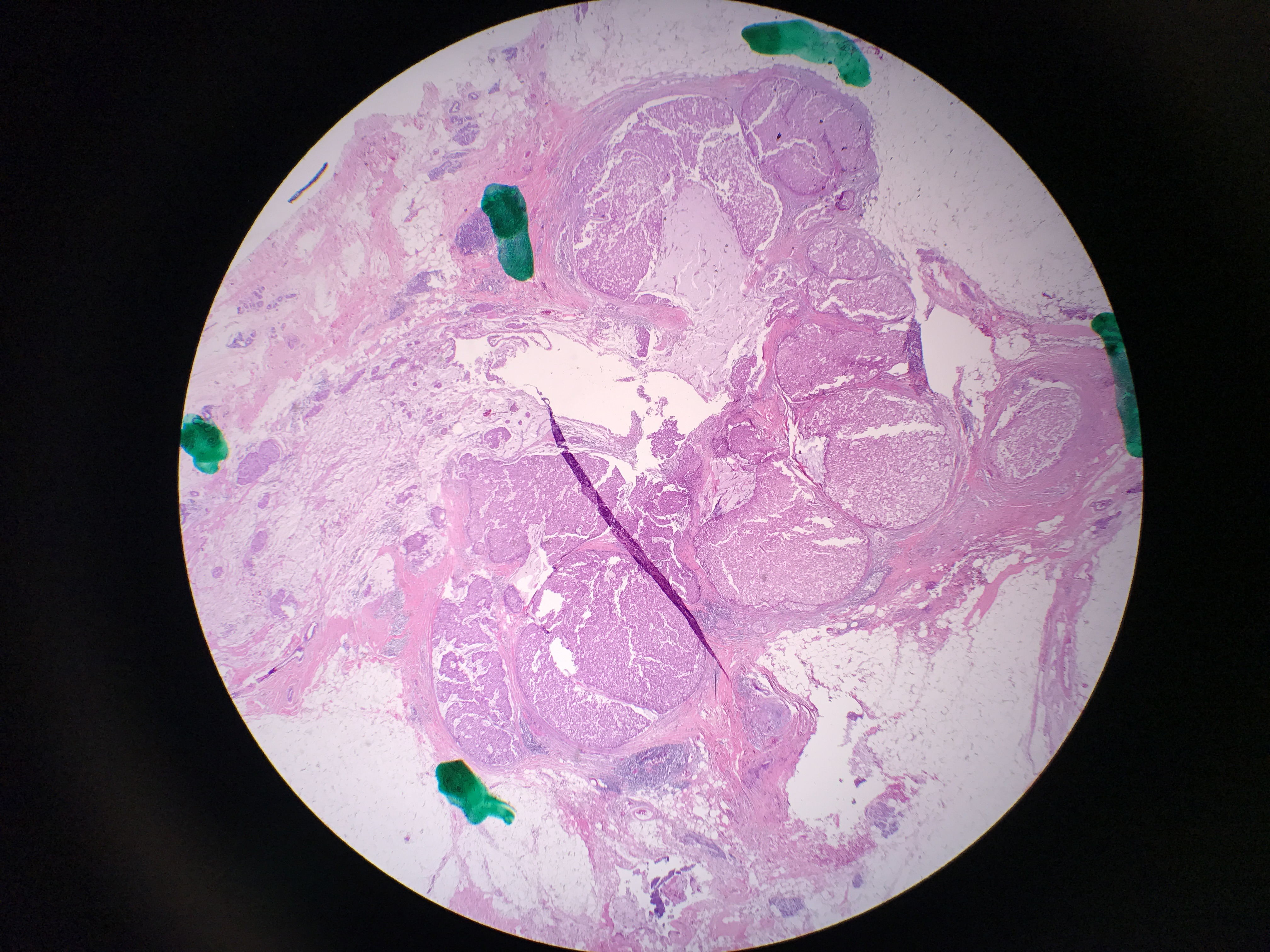
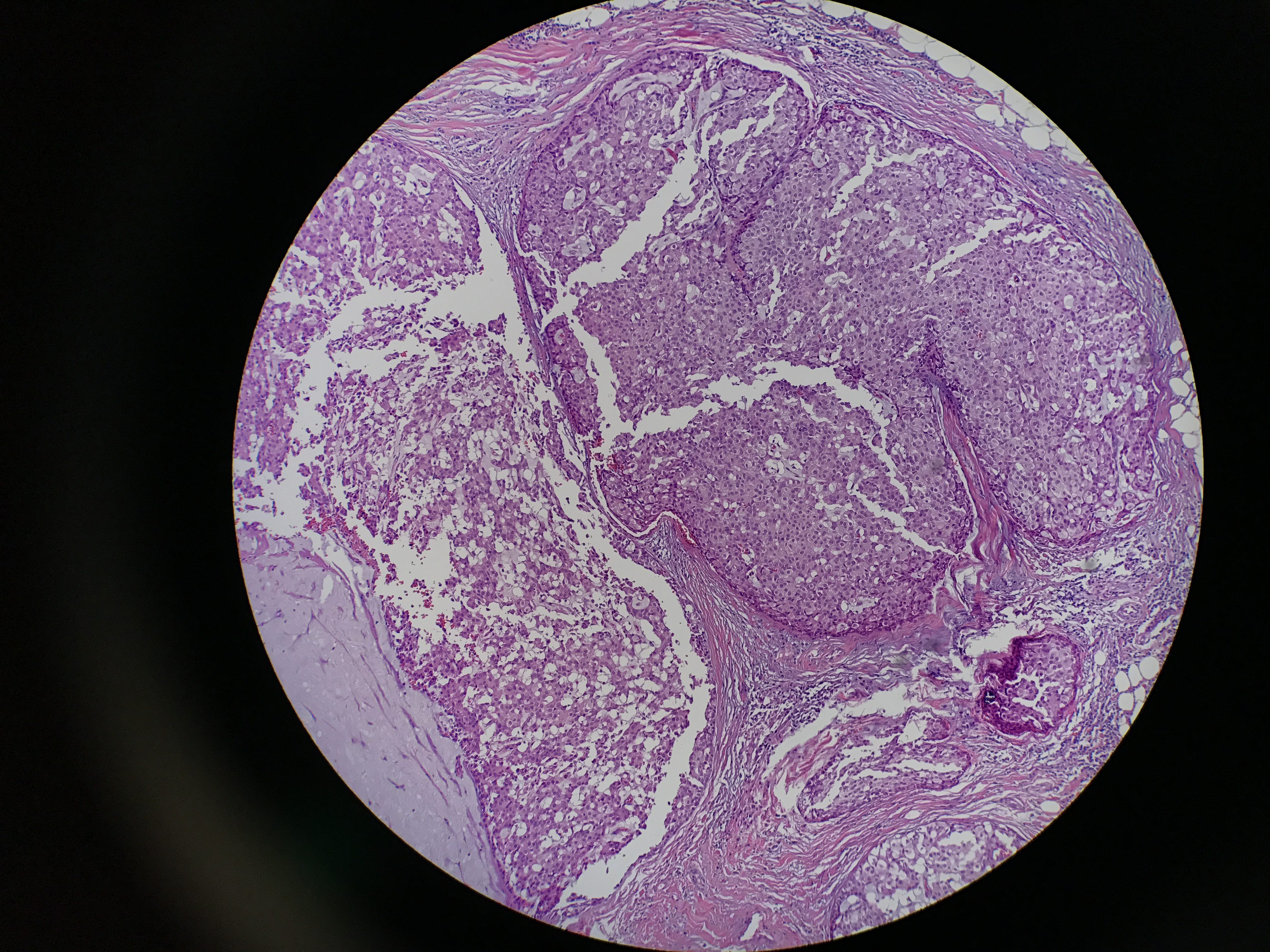
有个case想听听大家的意见。50s F left breast lumpectomy with sentinel lymph node biopsy. Biopsy was called at least DCIS. The entire lesion is 11 mm. 1 sentinel node is negative for carcinoma.
孔祥田(Max)*Sacramento*CA] 05-30 04:13
孔祥田(Max)*Sacramento*CA] 05-30 04:14

孔祥田(Max)*Sacramento*CA] 05-30 04:14
孔祥田(Max)*Sacramento*CA] 05-30 04:14
孔祥田(Max)*Sacramento*CA] 05-30 04:14
孔祥田(Max)*Sacramento*CA] 05-30 04:14
孔祥田(Max)*Sacramento*CA] 05-30 04:14

孔祥田(Max)*Sacramento*CA] 05-30 04:14
孔祥田(Max)*Sacramento*CA] 05-30 04:15
孔祥田(Max)*Sacramento*CA] 05-30 04:15
孔祥田(Max)*Sacramento*CA] 05-30 04:15
孔祥田(Max)*Sacramento*CA] 05-30 04:18
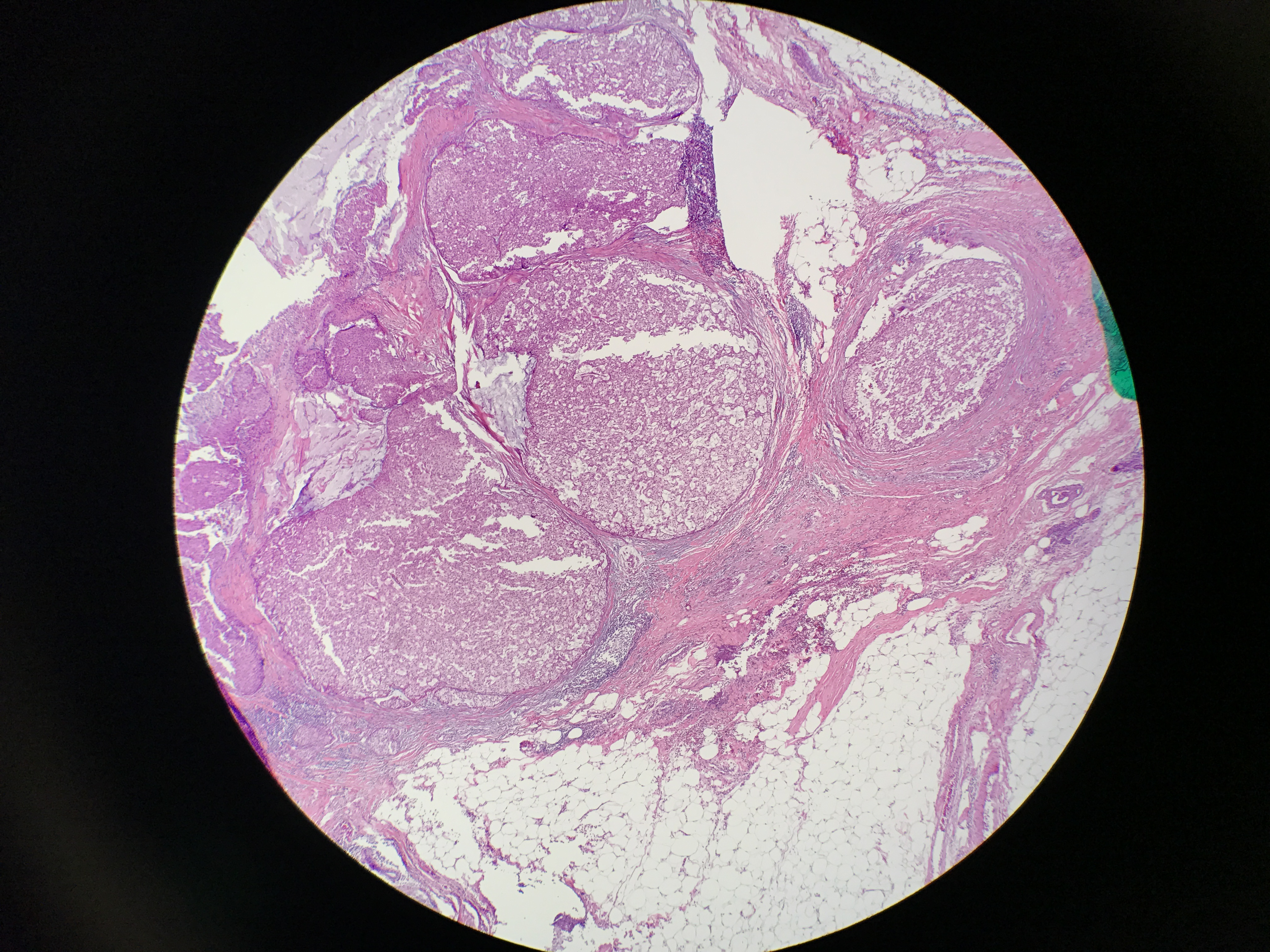
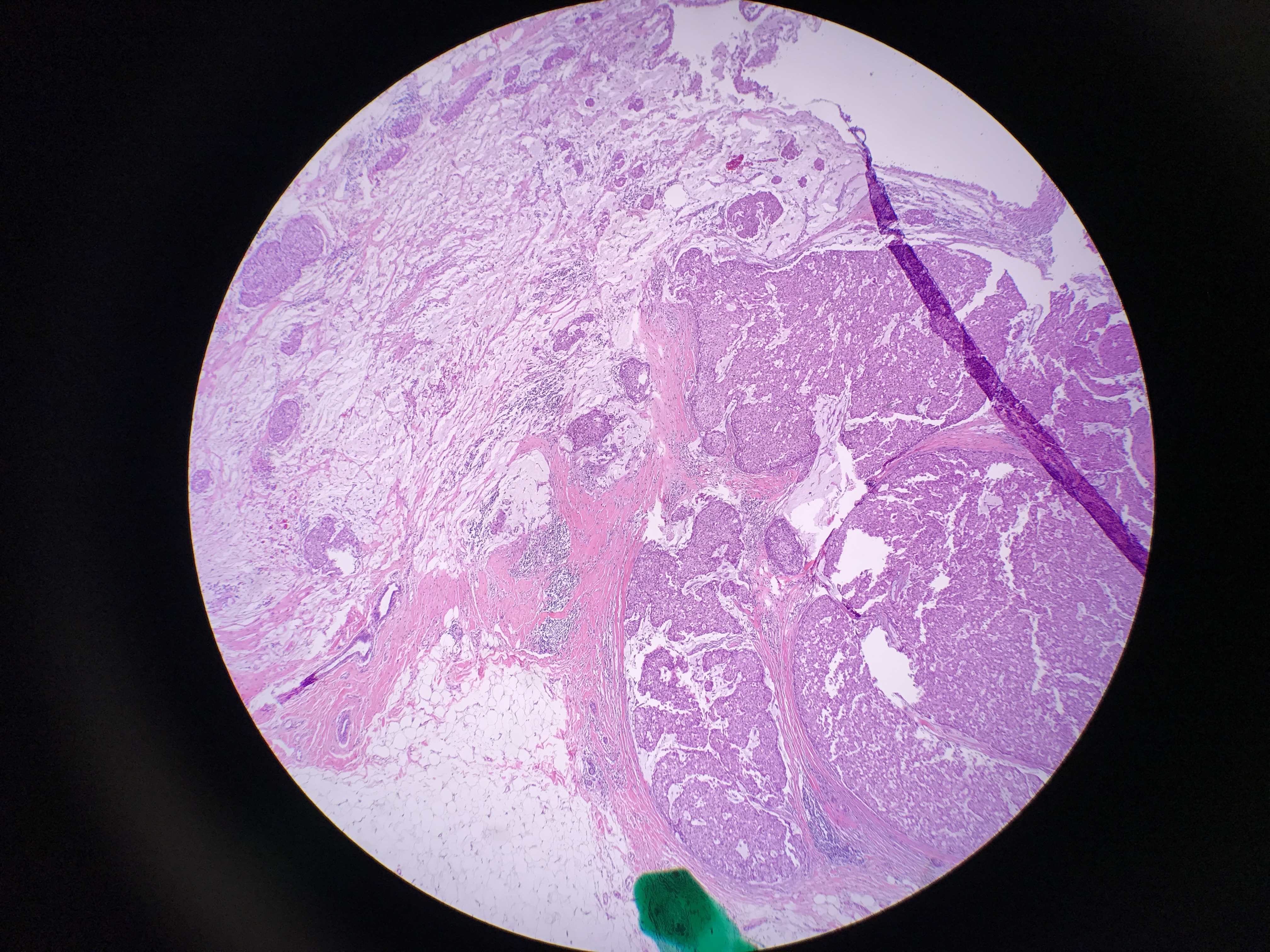
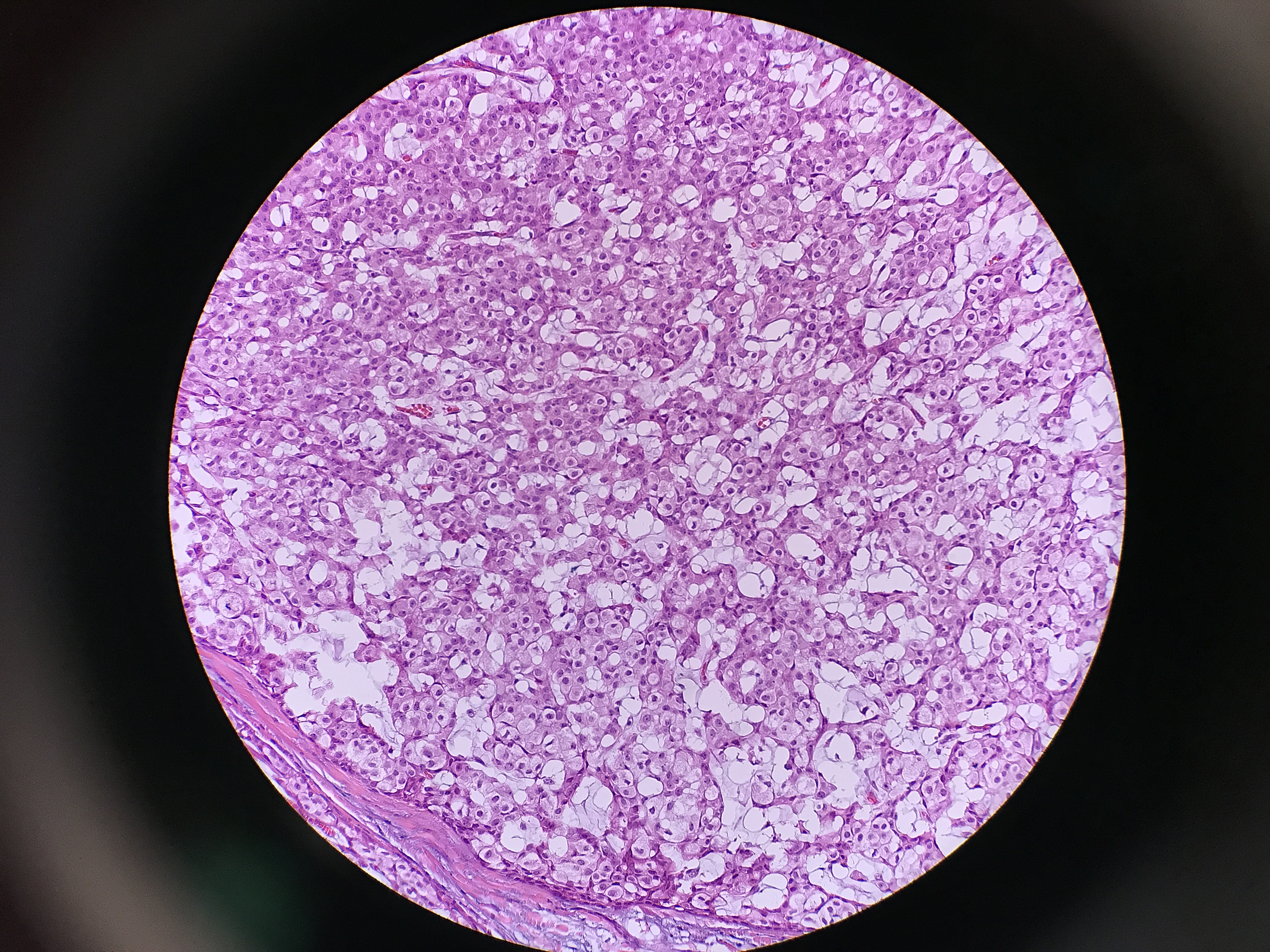
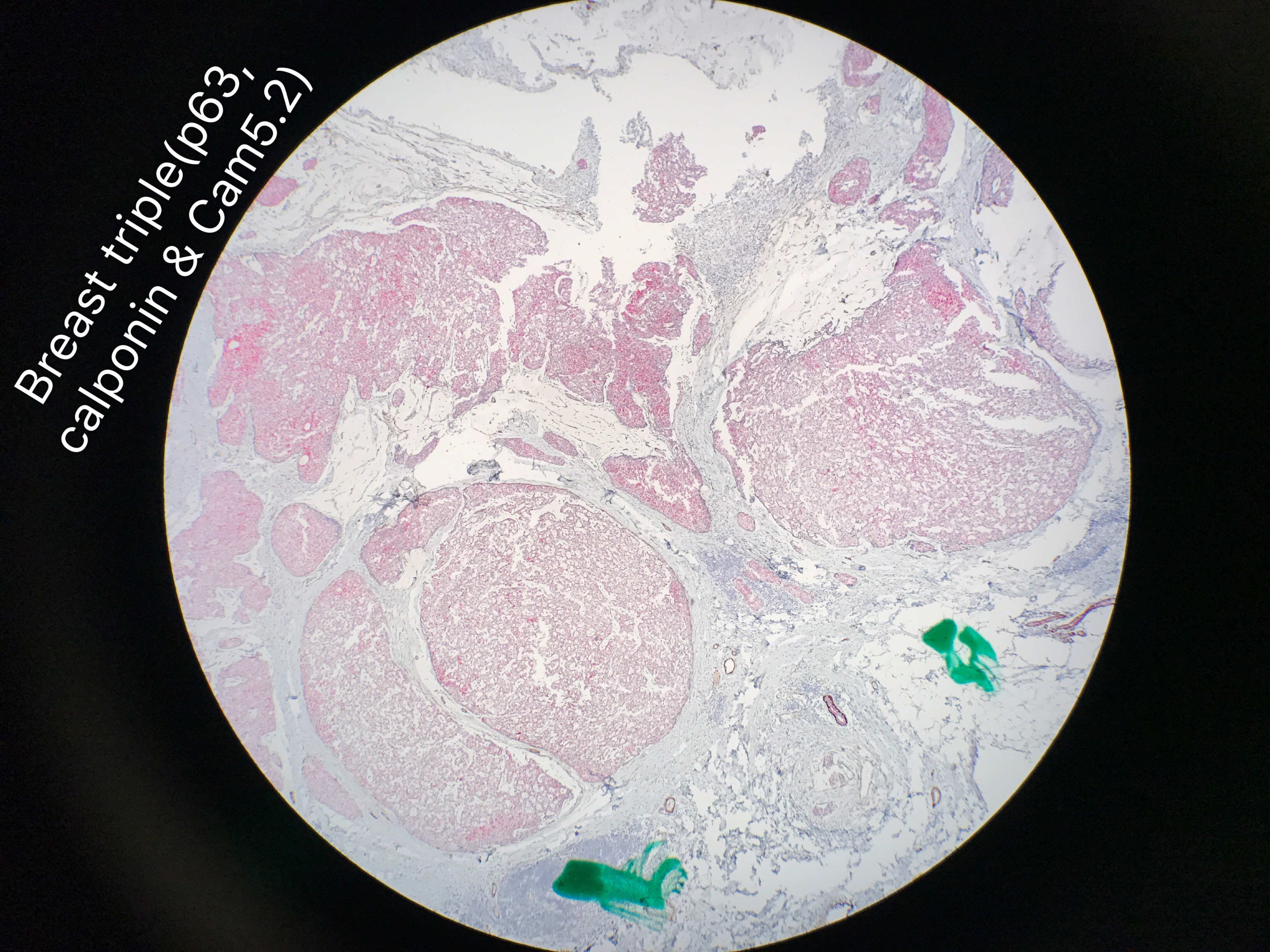
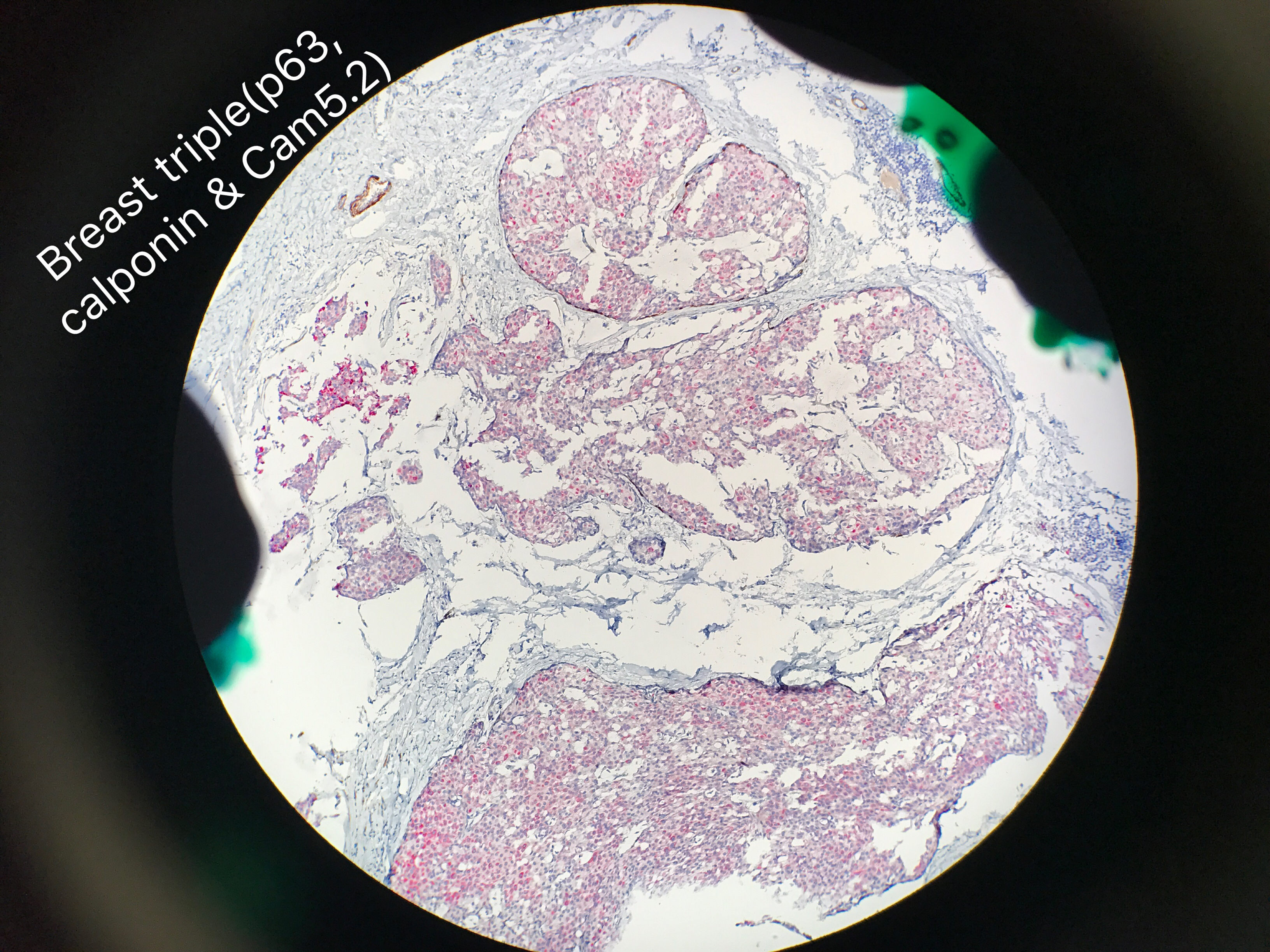
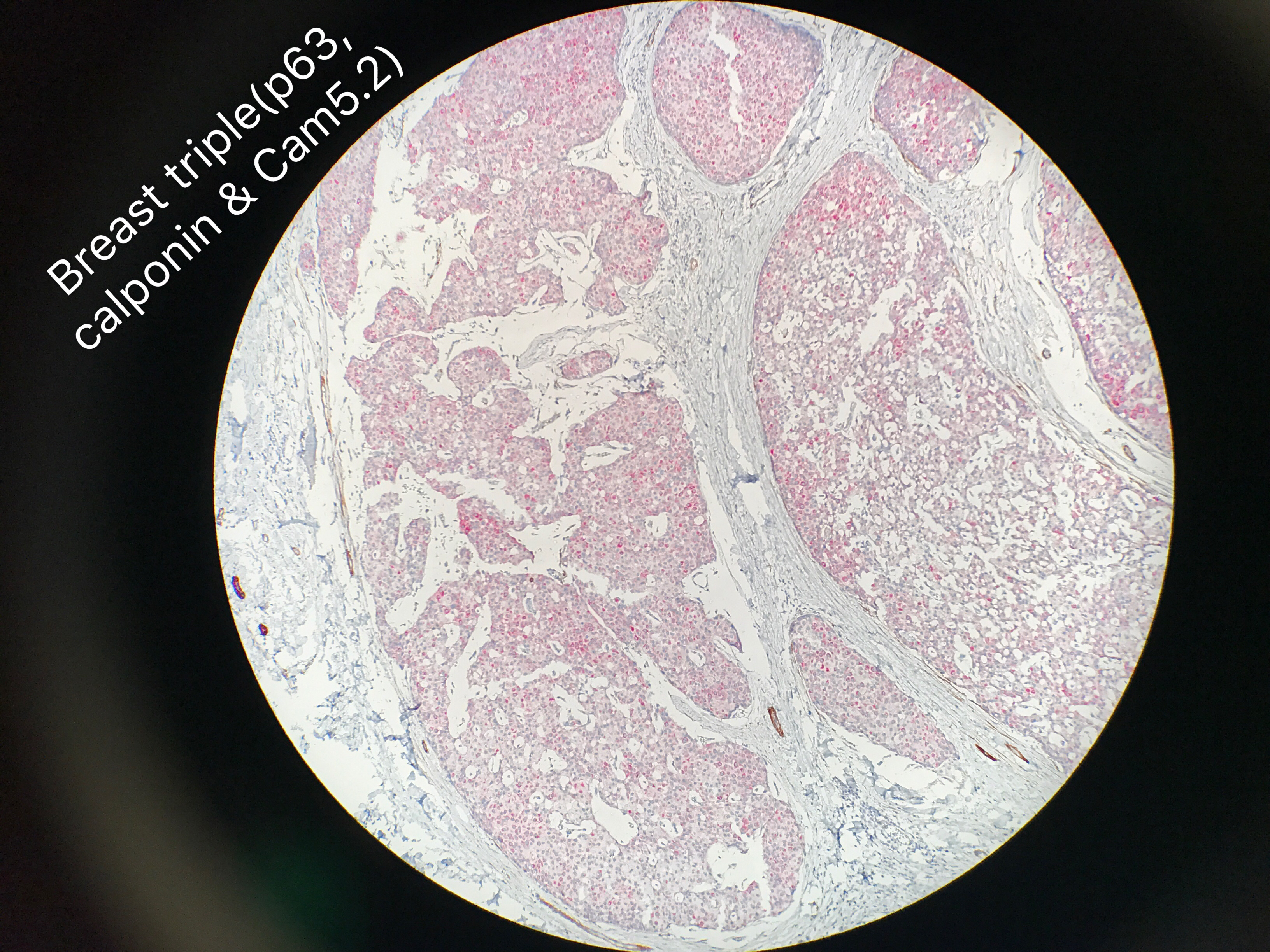
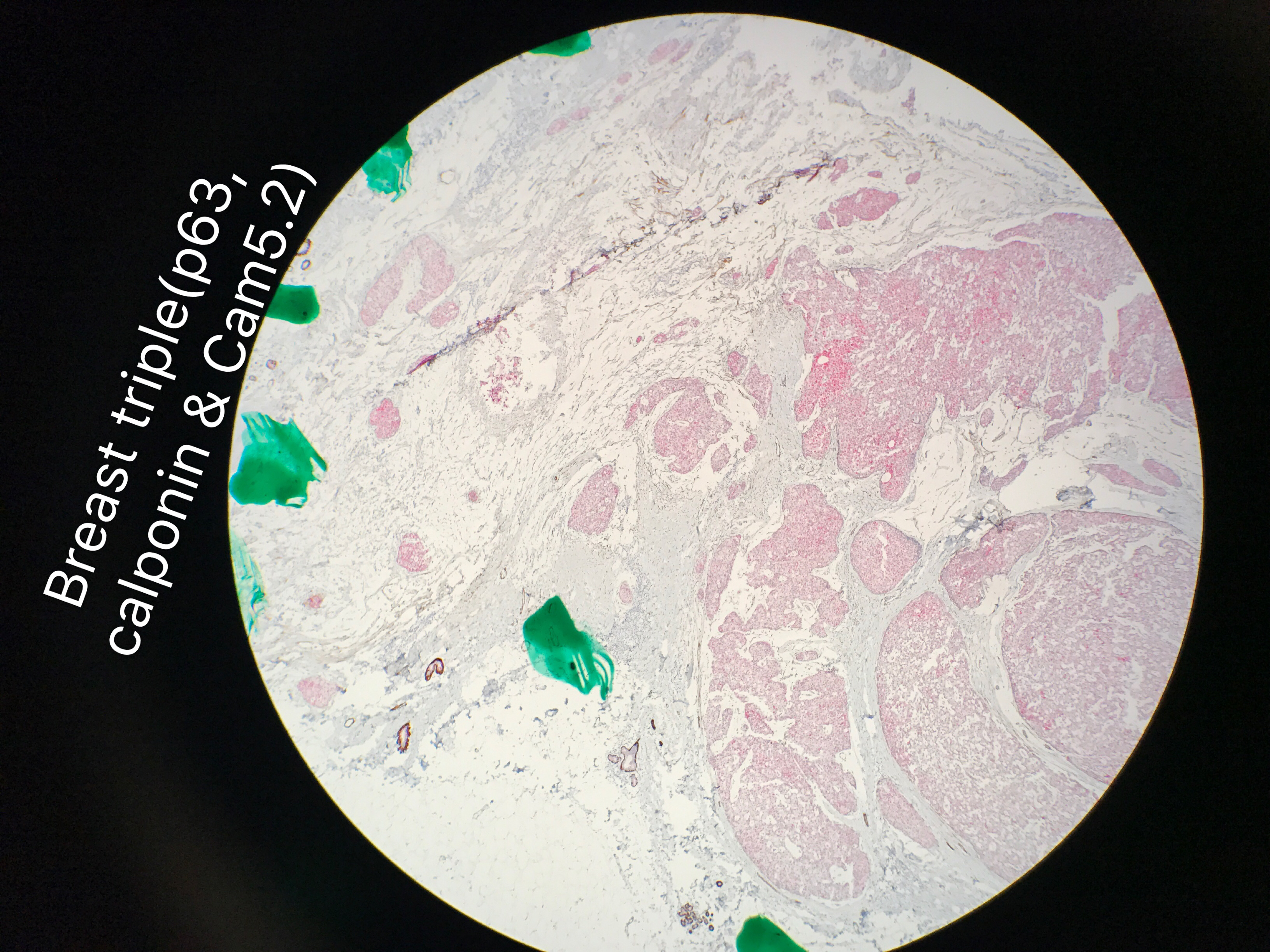
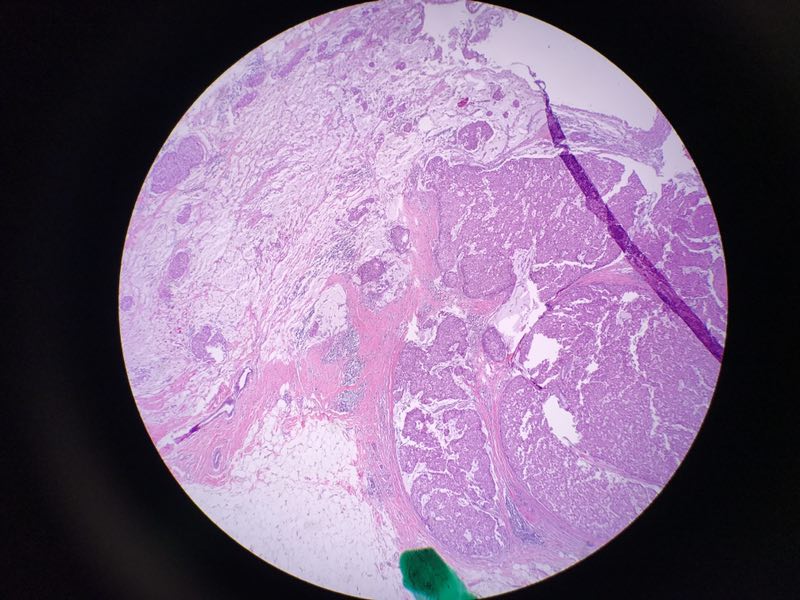
Patchy myoepithelial cells seen in small areas between the black dots on picture 7 and 9. Other areas lost the myoepithelial cells. There is myxoid stromal background. This is the only focus with lesion and bx clip.
孔祥田(Max)*Sacramento*CA] 05-30 04:21
Small nests seen in pictures 1, 4 and 11. Those nests seem in the bx track.
孔祥田(Max)*Sacramento*CA] 05-30 04:23
I personally feel the entire lesion is solid papillary carcinoma associated with adjacent DCIS. The nests in needle tract are artifact to me, not real invasion. Any objection or suggestions? Thanks

Andy K 05-30 05:02
@孔祥田(Max)*Sacramento*CA] This is an interesting case. I think the whole thing is invasive cancer, likely composite or collision tumor. You may have to run neuroendocrine makers to prove SPC. There is mucinous carcinoma as well, easily confirmed by mucicarmine. I think there's secretory component as well. You may do S100 to confirm it.

Wei Shi-UAB 05-30 05:30
@孔祥田(Max)*Sacramento*CA] @Andy K I would call it mucinous ca + spc, unless you prove that's not mucin. SPCs don't have to express neuroendocrine markers, although they often do.

李国霞上海 05-30 05:46
学习中:黏液背景中漂浮的那些巢,周围还有肌上皮吗?孔老师?如果那些巢周围没有肌上皮,考虑浸润性癌,看看细胞异型性和核级,核级低的,可以考虑黏液癌,核级高一点的,可以考虑浸润性导管癌伴黏液分泌。那些大巢好像SPC,神经内分泌标记阳性更好,阴性也不影响诊断SPC吧。

赵澄泉UPMC 05-30 06:09
赵澄泉UPMC 05-30 06:26
同意大家分析。这图左上细胞团一定是侵润癌。本例可能原来是SPC,进展成浸润。SPC与分泌粘液的癌常併生。神经内分泌染色无意义。此例最难的和可有争议的是如何测量浸润癌大小,以决定分期的问题。如有明显多处明显浸润,在实际工作中我可䏻按整个病变做为癌大小,1.1 cm. 诊断:浸润性导管癌伴局粘液,组织学2级(T-3; N-2, M-1; 总分6/9),癌大小为1.1 cm; SPC. 备注分析浸润癌起源于SPC.












