| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B4350卵巢肿瘤07年剔除,16年多部位复发
| 性别 | 女 | 年龄 | 42 | 临床诊断 | |
|---|---|---|---|---|---|
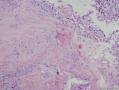
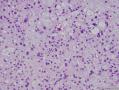
| 一般病史 | 患者07年行超声检查发现盆腔右侧一大小约6.9×3.8cm的不均质中等回声,边界不规则,尚清晰,内可见小囊状无回声区,大小约1.3×1cm,与右卵巢相邻,不易分辨;于腹腔镜下行右卵巢囊肿剔除术,术中见右卵巢表面有一大小8×8×7cm的肿物,与周围无粘连,活动度好,随即完整剥除肿物,术中见无腹水,肝、胆、胃肠均未见异常。今年患者因经期延长再次就诊,刮宫病检示子宫内膜复杂性增生,遂行全子宫+双附件切除术,术中发现双侧卵巢增大,部分网膜、肠管与盆壁粘连,全腹无明显肿块,无腹水。患者双侧髂窝包块,一并摘除送病检。 | ||||
| 标本名称 | 07年右卵巢肿物,16年双侧卵巢肿物,16年双侧髂窝肿物 | ||||
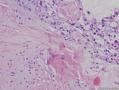
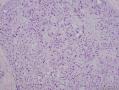
| 大体所见 | 07年右卵巢肿物:肿物大小8×8×7cm,切面灰白灰红,坏死明显,质中。 16年左卵巢:大小5.5×3.5×2.8cm,切面囊性,囊内有鲜红液体,囊壁厚0.1-1.3cm,并见一直径0.6cm的结节,灰黄、质硬。右卵巢:大小2×1.5×1.3cm,切面灰黄,见直径0.4-0.5cm的质硬结节状肿物2枚。 16年双侧髂窝肿物:灰白灰黄碎组织一堆,大小1×0.5×0.5cm。 | ||||
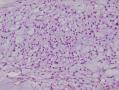
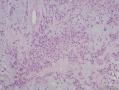
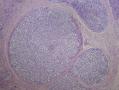
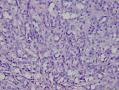
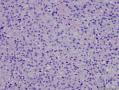
07年右卵巢肿物:

- 永不放弃
相关帖子
- • 卵巢肿瘤,如何报,请教诸位老师!谢谢!
- • 右侧卵巢肿瘤
- • 卵巢肿瘤分享1
- • 卵巢肿瘤分享3
- • 卵巢肿瘤分享4
- • 有趣的双侧卵巢肿瘤,请老师们看看
- • 女,69岁,右卵巢肿瘤
- • 64岁,卵巢肿瘤,求诊断
- • 女,34岁,卵巢肿瘤
- • 右卵巢肿瘤,交界还是恶性?
-
本帖最后由 小雪初晴 于 2016-08-26 20:58:28 编辑
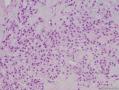
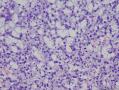
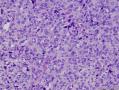
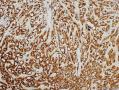
16年髂窝肿物:

- 永不放弃
CDK4阳性,MDM2阳性,似乎提示脂肪内容。但是,HE形态不支持,S100只有散在阳性,还有一个特点可能大家没有注意到,脂肪细胞和脂肪肿瘤Ki67呈胸膜/胞质阳性。
HE形态更像微囊性间质肿瘤,我们最近有一例,杨文涛教授在华夏病理十周年会议上讲过,它的免疫组化特点是CD10弥漫阳性,β-catenin 胞质+胞核阳性,可以试做一下。必要时请专家会诊。
-
www810910: 有些区域好像是有脂肪母细胞样细胞,关键是S100也不支持~2016-08-26 23:07

华夏病理/粉蓝医疗
为基层医院病理科提供全面解决方案,
努力让人人享有便捷准确可靠的病理诊断服务。
Microcystic stromal tumor of the ovary: report of 16 cases of a hitherto uncharacterized distinctive ovarian neoplasm
Am J Surg Pathol
Irving, J. A. Young, R. H.
We have encountered 16 ovarian neoplasms of probable stromal origin whose most distinctive feature is microcystic change, which is usually conspicuous. On the basis of our extensive experience with ovarian tumors, the neoplasm is unique and warrants separate categorization; we have elected to designate it "microcystic stromal tumor" because of its most striking feature. The patients ranged from 26 to 63 (mean 45) years of age and typically presented with a pelvic mass. Hormonal manifestations were possibly present in only 2. All tumors were unilateral with a mean size of 8.7 (range: 2 to 27) cm and none had evidence of extraovarian spread. The tumors were solid-cystic (11 cases), solid (3 cases), or predominantly cystic (2 cases). The solid component was usually firm and tan or white-tan, but in 1 case was yellowish; soft foci were present in 3 cases and small foci of hemorrhage, necrosis, or both, in 3. On microscopic examination the appearance of the tumors varied according to the relative prominence of their 3 fundamental components: microcysts, solid cellular regions, and fibrous stroma. Microcysts dominated in 9 cases, were roughly equal to noncystic morphology in 5 cases and were minor in 2. The microcystic pattern was characterized by small rounded to oval cystic spaces, in areas coalescing to larger irregular channels; intracytoplasmic vacuoles were also frequently present. The solid cellular areas were usually focally intersected by fibrous bands and hyaline plaques reminiscent of thecoma. The cells contained moderately conspicuous finely granular, lightly eosinophilic cytoplasm, with generally bland, round to oval or spindle-shaped nuclei with fine chromatin and small indistinct nucleoli. Foci of bizarre nuclei were, however, present in 10 cases. Mitotic rate was low in all cases, ranging from 0 to 2 mitoses/10 high-power fields. Immunohistochemical results were as follows: CD10, 16/16 cases positive; vimentin, 16/16 cases positive; inhibin, 1/16 cases weakly positive; calretinin, 1/16 cases positive; cytokeratin, 4/16 cases focally positive; and epithelial membrane antigen, 0/16 cases positive. Microcystic change can be observed in a wide variety of ovarian tumors and the broad potential differential diagnosis is discussed in the text. For tumors which have been well sampled and exhibit (1) a microcystic pattern and regions with lobulated cellular masses with intervening, sometimes hyalinized fibrous stroma, (2) an absence of morphologic features enabling any other specific diagnosis in the sex cord-stromal category, (3) an absence of epithelial elements, and (4) an absence of teratomatous or other germ cell elements, we propose the designation "microcystic stromal tumor." The characteristic immunophenotype is CD10/vimentin+/epithelial membrane antigen-, with focal cytokeratin-positivity in one-quarter of cases; inhibin and/or calretinin are usually negative. Seven patients with available follow-up are without evidence of disease at a mean of 4.25 years (range: 1.5 to 12.5 y) from the time of initial diagnosis. These tumors, to date, have occurred over a wide age range in postpubertal females, are characteristically unilateral, and confined to the ovary at presentation. They represent, in addition to the sclerosing stromal tumor (segregated out 3 decades ago), a distinctive subtype of ovarian tumor, likely also belonging to the stromal category based on current evidence.
-
城北: 首次的16例报道,总结了免疫组化特征2016-08-30 15:21
-
www810910: 学习了,谢谢城北哥~来自Android 2016-08-30 15:29

知之者不如好之者,好之者不如乐之者。(语出幽梦影)
Microcystic stromal tumor (MCST) is a recently described subtype of ovarian tumor characterized by prominent microcystic histologic pattern and diffuse immunoreactivity for CD10 and vimentin. However, its pathobiology, particularly its histogenesis, remains largely unclear. Here, we report 2 cases of ovarian MCST, in which we have performed extensive histologic, immunohistochemical, and genetic investigations to determine its distinct nature among ovarian neoplasms. The patients were 32 and 41 years of age. Both tumors were solid and cystic masses involving the right ovary. Microscopically, tumor cells with generally bland, round-to-ovoid nuclei grew in microcystic, macrocystic, and solid patterns. Intervening thick fibrous stroma was observed. Immunohistochemically, tumor cells were diffusely and strongly positive for CD10, vimentin, and Wilms tumor 1. Furthermore, we detected aberrant nuclear expression of β-catenin protein in both cases. Of interest, mutation analyses revealed the presence of an identical point mutation, c.98C>G, in exon 3 of β-catenin (CTNNB1) in both tumors. This is an oncogenic mutation that causes replacement of serine with cysteine at codon 33, leading to the loss of a phosphorylation site in the β-catenin protein. The results of this study strongly suggest that dysregulation of the Wnt/β-catenin pathway plays a fundamental role in the pathogenesis of ovarian MCST. Finally, by comparing the immunophenotype of MCST with its histologic mimics and other ovarian sex cord-stromal tumors, we were able to identify unique features of MCST and a panel of markers useful in differential diagnosis.

知之者不如好之者,好之者不如乐之者。(语出幽梦影)
-
本帖最后由 城北 于 2016-08-30 15:43:51 编辑
-
小雪初晴: 谢谢城北哥的帮助查找文献和回复,本例现在的免疫表型:CD10+,β-catenin+,CD99呈特异性的核旁逗点状+,是符合卵巢实性假乳头装肿瘤的,在微信群里也有很多老师提出该诊断。2016-09-01 12:40

知之者不如好之者,好之者不如乐之者。(语出幽梦影)
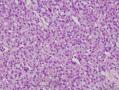
感谢各位老师的回复,本例现在的免疫表型:CD10+,β-catenin+,CD99呈特异性的核旁逗点状+,是符合卵巢实性假乳头装肿瘤的,在微信群里也有很多老师提出该诊断。其实通过镜下观察,本例形态更符合卵巢微囊性间质性肿瘤(MCST),但是,唯一纠结的是,患者时隔9年双侧卵巢复发且双侧髂窝转移,与MCST所报道的生物学行为不符。还有一部分老师们的意见是卵巢Sertoli-Leydig细胞肿瘤(SLCT),但免疫表型不符合之处是本例inhibin和CD56均阴性。
至今我们仍然无法做出一个明确诊断,还请各位老师继续关注和讨论,谢谢!
-
www810910: 有意思的病例,学习~来自Android 2016-09-02 17:00
-
wuxin: 感谢提供这么好的病例学习,并详细的解读。2016-09-03 15:16

- 永不放弃
-
07年的肿物第一眼印象是卵巢的微囊型间质瘤,细胞小,核圆形一致,有微囊结构。

- 优秀的医生相信自己看到的!
此病例已撰写为病例报告,发表在Human Pathology杂志,链接:https://www.ncbi.nlm.nih.gov/pubmed/29458068
感谢各位网友的关注!

- 永不放弃