| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
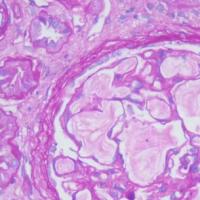
- 甲状腺内小结节,鳞化?
-
liangjinjun 离线
- 帖子:2328
- 粉蓝豆:2
- 经验:2457
- 注册时间:2007-08-07
- 加关注 | 发消息
-
shihong4699 离线
- 帖子:1024
- 粉蓝豆:43
- 经验:2917
- 注册时间:2009-01-20
- 加关注 | 发消息
-
本帖最后由 wang4160 于 2014-06-27 17:01:03 编辑
非常好的病例!建议版主顶置,并讨论!!
非常想向Warthin瘤样乳头状癌上靠,而且结构上很像乳头状癌,但没有诊断经验!
ABSTRACT:Warthin-like tumor of the thyroid is a recently described rare variant
of thyroid papillary carcinoma. h e distinguishing histological feature
of this variant is papillary foldings lined by oncocytic neoplastic cells
with clear nuclei and nuclear pseudoinclusions, accompanied by
prominent lymphocytic infiltrate in the papillary stalks. Its prognosis
has been reported to be almost similar to conventional papillary
carcinoma. In this case series, we report four cases with Warthin-like
papillary carcinoma of the thyroid, diagnosed at Dokuz Eylul
University Faculty of Medicine Department of Pathology in 2008 and
2009. h ree patients were female. h e mean patient age was 39 years
(range, 20-56) and the mean tumor size was 1.7 cm (range, 0.9-2.0 cm).
All of the cases had lymphocytic thyroiditis in the background. None
of the tumors showed lymphovascular invasion. h e patients are free
of any recurrence and/or distant metastasis with a mean follow-up
of 25 months. h is rare variant of thyroid papillary carcinoma with
distinct histopathological features should be indicated in pathology
reports. Further studies and long-term follow-up of patients are
needed to highlight the biological behavior of this variant.
TheWarthin-like variant of papillary thyroid carcinoma was
first described in 1995 by Apel et al. [2] and represents a
rare variant of PTC, with approximately eighty cases having
been reported in literature to date [1]. Apel et al. chose
the name “Warthin-like tumor” because of its histological
resemblance to papillary cystoadenoma lymphomatosum or
Warthin tumor of the salivary glands.
Patients affected by WaLPTT have similar demographic
and clinical characteristics to those affected by PTC. Table 1
shows these characteristics, as reported in the most consis-
tent series published to date, excluding case reports [2–7].
WaLPTT typically arises at an earlier age, as compared to
PTC, and there is also a stronger predominance of females.
Among the 54 patients reviewed, the mean age was 50
years and there were only five males (9%). The clinical
presentation is the same as that for other differentiated
thyroid tumors: absence of signs and symptoms when the
lesions are single, small, and deep; palpablemasses, glandular
swelling, and swallowing and/or phonatory alterations for
larger, superficial, and/or multiple lesions. Signs, symptoms,
and alterations in thyroid function related to thyroiditis or
goitre may be also present. Furthermore, features of US and
CT imaging of WaLPTT are identical to those for PTC. As
a consequence, diagnosis of WaLPTT cannot be based on
clinical and imaging data alone.
FNA may be useful in this regard, but its role in the
diagnosis ofWaLPTT is not yet clear. Generally, it is possible
to appreciate the presence of groups of follicular cells and
papillary fragments against a background of lymphocytes
and plasma cells, which infiltrate the fibrovascular cores.
Oncocytic cells are often admixed with lymphocytes. The
nuclear characteristics of tumoral cells are generally those
of PTC (nuclear chromatin clearing, membrane thickening,
grooves, and pseudoinclusions) and oncocytes (round nuclei
with coarse chromatin and prominent nucleoli) [5]. Such
patterns suggest PTC or lymphocytic thyroiditis, or both.
Indeed, these were the most frequent diagnoses in the
literature on patients affected byWaLPTT. Baloch and LiVolsi
report data on seven FNAs; there were four diagnoses of
PTC, two of lymphocytic thyroiditis and one of atypical
cells [5]. In the series of D’Antonio et al., all patients
underwent FNA and two of them had a diagnosis of PTC;
in one case, the results of FNA were inconclusive [4]. In
our case and those of Amico et al., Sarkady et al., and
Lam et al., the preoperative diagnosis based on FNA was
PTC or thyroiditis [1, 8, 9].FNAisprobablymoreusefulfor
the evaluation of cervical lymph node involvement, as in our
case, and for planning the appropriate surgical strategy and
multidisciplinary management.
The macroscopic appearance of WaLPTT is generally
that of a white-greyish, well circumscribed nodule, unen-
capsulated and confined to the thyroid gland. It may contain
cystic and/or haemorrhagic areas. Its mean size among the
54 reviewed patients was 1.5 cm (range 0.3 to 5 cm). To
our knowledge, only one paper has reported a WaLPTT
larger then 5 cm [1]. The color of the remaining thyroid
parenchyma generally ranges from red brownish to tan and a
variable number of nodules of different sizes may be present.
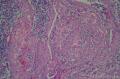
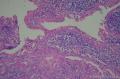
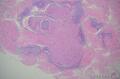
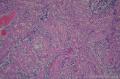
The histological diagnosis of WaLPTT is based on the
evidence of a morphological pattern featuring papillae lined
by oncocytic cells admixed with lymphocytes and sparse
plasma cells. The distinctive feature is the lymphocytic infil-
tration of the stalks of the papillae. Furthermore, it is possible
to observe cysts or a small number of tall cells. Vascular
and capsular invasions are rare. Differential diagnosis must
be conducted with other variants of papillary cancer with
similar morphology, such as Hurthle cell carcinoma (HCC)
and tall cell carcinoma (TCC). The former usually lacks
lymphoplasmacytic infiltrates and is rarely associated with
lymphocytic thyroiditis [2, 5]; the latter is characterized
by a papillary structure with elongated oncocytes, with a
height that is more than twice their width, and by neoplastic
aggressiveness with more frequent vascular, capsular, and
nodal invasion [10].
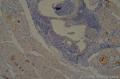
Theroleofimmunohistochemistryindifferential diag-
nosis with Hurthle cell and tall cell carcinomas is limited.
Indeed, in our case it was not necessary for diagnosis as
the morphological pattern was clear. Intense staining for the
following markers has been reported in literature: galectin-3,
HBME-1, CK19, TTF-1, thyroglobulin, EMA, AE1/AE3,
S-100 protein, cyclin D1 and UCHL1, CD3+, CD20+,
and CD79+ (for the lymphocytic population). Ostrowski
and Merino believe that CD15 immunostaining represents
a distinctive characteristic of tall cell carcinomas and a
predictive factor for advanced stage or poor prognosis [11].
Nevertheless, this marker was also found in WaLPTT, which
has a better prognosis than TCC.
The neoplastic behaviour of WaLPTT seems to be similar
or even better than that of classical PTC. Vera-Sempere et al.
hypothesized that it is a hybrid of TCC and HCC and
some immunohistochemical evidence supports this theory
[12]. Short- and long-term prognosis seems to be excellent.
Lam et al. describe a case of a 74-year-old Chinese woman
affected by WaLPTT with dedifferentiated (anaplastic) area
[9]. She had a 3.5 cm PTC of the right lobe with ipsilateral
recurrent laryngeal nerve involvement; a supraclavicular
lymph node was shown by FNA to be metastatic. The patient
refused any treatment for three years, but agreed to undergo
surgery when her condition worsened. She underwent pal-
liative surgery and died 15 months later. This case seems to
have involved the natural evolution of an advanced anaplastic
thyroid carcinoma (with areas of WaLPTT) that remained
untreated for a long time, rather than a typical WaLPTT.
Elsewhere, Amico et al. reported a case of a 6 cm WaLPTT
with less than 5% of the tumor area being occupied by
anaplastic tissue in a 79-year-old woman with laterocervical
lymph node metastasis [1]. The patient promptly underwent
surgery and was alive without evidence of disease 23 months
later. It is probable that in such situations the anaplastic
component, even when it represents a small percentage of
the overall tumor area, dictates the prognosis, which may be
poor when appropriate treatment is not provided.
Other cases of cervical nodal metastasis have been
reported in literature, but such events are generally rare
[3, 8]. Among the 54 cases reviewed here, only 12 (22%) had
lymph node metastasis, which represents an incidence lower
than that for traditional PTC. Prognosis was favourable in
almost all cases, but follow-up times were generally short,
with only a few cases being followed for more than 3 years.
The most reliable explanation for the low rates of nodal
involvement and favourable prognosis in WaLPTT is the
presence of lymphatic tissue within the tumor, which seems
to contrast and restrain neoplastic progression and diffusion.
The therapeutic management of patients with WaLPTT
is similar to that of patients with PTC and depends
substantially on the disease stage and the presence of neg-
ative prognostic factors such as familiarity, history of neck
irradiation, and syndromic endocrine disease. The diagnosis
of WaLPTT is histopathological and generally based on
surgical specimens. This means that the therapeutic plan
for patients with WaLPTT must be assessed after surgery.
The reports reviewed in this paper are mostly pathological
and lack detailed data on postoperative treatments such as
radioiodine ablation and follow-up modalities. As the bio-
logical behaviour of WaLPTT is comparable to that of PTC,
postoperative management should also be identical. Further
surgery for completion of thyroidectomy or lymphadenec-
tomy, radioiodine ablation, and other treatments may be
employed in high-risk patients. Our patient underwent
postoperative radioiodine therapy due to evidence of residual
thyroid tissue and capsular invasion and is undergoing the
same postoperative follow-up and treatment program used
in patients with classic PTC.
4. Conclusions
Warthin-like papillary thyroid carcinoma is a recently
described variant of papillary thyroid cancer that is fre-
quently associated with lymphocytic thyroiditis.Morpholog-
ically, it resembles Warthin tumors of the salivary glands,
with T and B lymphocytes infiltrating the stalks of papillae
lined with oncocytic cells. Diagnosis is histopathological and
based on morphology rather than immunohistochemistry.
Surgical and postoperative management is identical to that
of classic differentiated thyroid cancer, while prognosis seems
to be favourable. Larger prospective long-term studies are
necessary to better understand the biological behaviour of
such tumors and their clinical and prognostic impact.