| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 女,57岁 肝外胆管肿物(最大径1.5cm)
1.肝外胆管癌 我国肝外胆管癌发生率近年渐增。
【临床要点】①多见于老年人(平均年龄>60岁),男性稍多。②与硬化性胆管炎、溃疡性结肠炎、胆总管囊肿、胆胰管异常结合和肝吸虫感染等有关。 ③多较小(≤2cm,可>5cm)、单发。④常较早出现梗阻性黄疸(可迅速进展或呈现波动)。⑤可右上腹痛、不适、体重下降、皮肤瘙痒、畏食、恶心呕吐等。⑥伴发胆管炎时可寒战、发热。⑦约半数病例的肿瘤位于上段胆管(左、右肝管和总肝管)癌,致肝内胆管扩张,胆囊不能触及,胆总管常塌陷;胆总管癌时,胆囊扩张,可触及,上段胆管明显扩张。⑧约半数病例的肝外胆管癌在因胆结石等行胆管切除的标本中发现。⑨TNM分期可确定肿瘤范围,与预后密切相关;对胆囊切除标本,病理诊断应报告分期情况。⑩预后较差。
【病理变化】
(1)肉眼病变:①肿瘤直径多≤2cm。②多发于上、中段胆管,晚期可累及全段胆管。③受累及管壁增厚、僵硬,灰白色。④分为:息肉型、结节型、硬化狭窄型和弥漫浸润型(有助于指导切除范围和评估预后);实际上除息肉型外,其他三型不易明确区分。⑤结节型、硬化狭窄型倾向于浸润周围组织而难以切除,弥漫浸润型则倾向于沿胆管长轴呈线状播散。⑥病程较长者,可继发胆汁性肝硬化。
(2)光镜病变:①主要为腺癌。②组织学类型与胆囊癌者相同。
硬化性胆管癌:①肝外胆管癌特殊类型。②始发于肝管连接处,累及一长段胆管树。③多分化较好,伴广泛纤维化;可分化很好(包括其转移瘤),以致难以诊断为恶性。④病变特征:同一腺体中的肿瘤细胞形态不一致,核、浆比值增加,核仁明显,浸润间质和神经,腺体围以同心圆状富于细胞的间质。 ⑤肝外胆管癌的活检取材(穿刺或胆管腔内取出物)较少,常难以检见肿瘤细胞浸润。
【病理鉴别诊断】①乳头状异型增生和乳头状瘤;②异位胰腺等。
2.其他 ①类癌;②囊腺癌;③癌肉瘤;④葡萄状横纹肌肉瘤;⑤恶性纤维组织细胞瘤;⑥黑色素瘤等。
摘自《临床诊疗指南(病理学分册)》

- 邓学田
-
本帖最后由 leanna 于 2012-09-07 16:35:53 编辑
同意9楼。
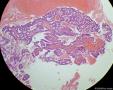
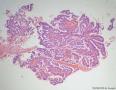
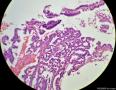
黏液柱状上皮围绕纤维血管轴心乳头状排列,局部上皮细胞黏液成分变少或消失,细胞核变圆,细胞极像紊乱。
诊断:(肝外胆管)分泌型乳头状瘤(腺瘤),若为多发则为乳头状瘤病(腺瘤病)。
此病常伴轻中度异型增生,是具有恶性潜能的交界性肿瘤,有癌变倾向。
Biliary Papillomatosis
Clinical and Pathologic Features.—Biliary papillomatosis is a rare disorder that was first described by Caroli and colleagues in 1959 (13). It is characterized by multiple and recurrent papillary adenomas in the biliary tract. The extrahepatic bile ducts are involved in the majority of cases. The intrahepatic bile ducts, cystic duct, gallbladder, and pancreatic duct may also be affected. Occasionally, the process involves only the intrahepatic ducts (14).
The majority of patients present for medical attention between the ages of 50 and 60 years, and men and women are equally affected (7). Patients present with signs and symptoms of biliary obstruction that is often complicated by cholangitis (15). Complete surgical excision of biliary papillomatosis is difficult and local recurrence is common. Some authors regard this lesion as a form of low-grade intraductal carcinoma (7). Papillomatosis has a greater potential for malignant transformation than a solitary adenoma.
Biliary papillomatosis is histologically characterized by biliary duct dilatation and multiple papillary adenomas. The epithelium of the papillary adenomas is composed of mucin-secreting columnar or cuboidal cells with basal nuclei. A fibrovascular core supports the epithelium (Fig 9a). Complex glandular structures (representing in situ carcinoma) and occasionally papillary carcinoma may be present.
At gross inspection, the affected bile ducts are dilated. The bile duct walls may appear thickened and fibrotic. Intraluminal mucin may be visible. The papillary adenomas are typically tan, soft, and friable polyps (14) and usually do not demonstrate gross invasion of the bile duct wall (Fig 9b). Tumors that produce a significant amount of mucin may have a doughy or jellylike consistency (16).

名称:图1
描述:Figure 9a. Biliary papillomatosis in a 65-year-old man who presented with jaundice and sepsis. (a) Photomicrograph (original magnification, ×2; H-E stain) shows multiple papillary projections lining the bile duct wall.
文章检索号 PMID: 11896229

- pathology