| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- B71(ZT)臀部包块
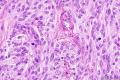
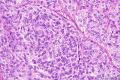
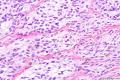
本例有考虑痣样恶黑的,考虑透明细胞肉瘤者占多数,也有考虑细胞性蓝痣伴有(轻度)非典型性或非典型细胞性蓝痣
到底是啥呢?
它们之间如何鉴别诊断,本例会牵扯到很多混淆的问题,因为免疫组织化学上面3个表达是一样的。IHC几乎没啥帮助。我看到这个病例的答案后十分疑惑,颠覆了本人的既有认识,查阅文献后感觉这可能是很有争议的病例,也许只有分子遗传学才能最终搞定。本例需要进一步讨论,有高手愿意指出来吗?答案就在上面的一个中,3选1,当然原上传者的答案不一定就100%正确,但是对于学习新知识和讨论很有帮助
希望大家踊跃参与讨论
-
本帖最后由 TK1905 于 2012-05-08 23:43:59 编辑
这例不是透明细胞肉瘤,如何鉴别下面的3个诊断?
细胞性蓝痣
软组织透明细胞肉瘤
痣样恶黑
本例最终诊断:细胞性蓝痣
原作者:
Phillip H McKee Wrote:
Melanocytic lesions continue to be a problem for most of you. This is nothing more than a cellular blue nevus. There is no significant pleomorphism and I deliberately chose a field with two mitoses to catch out the unwary. Although I do not like the term "atypical" as applied to melanocytic lesions personally believing that in the overwhelming majority of cases one should be able to determine whether a lesion is a nevus or a melanoma, if you do use the term atypical cellular blue nevus, there is insufficient atypia. The presence of mitositic activity is anticipated in most cellular blue nevi.
软组织肿瘤第5版上面讲到鉴别诊断:
The distinction of clear cell sarcoma from other melanin-producing lesions can be more problematic and may require correlation of the histologic, clinical, and molecular data. In general, clear cell sarcomas originate in deep structures, rarely involve the dermis, and have a predominantly and relatively uniform spindle-cell appearance that contrasts with the epithelioid appearance of nodular melanomas. However, in ambiguous situations, molecular genetic analysis is highly recommended since the t(12;22) that characterizes clear cell sarcoma has not been identified in malignant melanoma. Cellular blue nevus can occur in a similar age and location and have certain common histologic features including spindled cells and giant cells with clear cytoplasm. Cellular blue nevi typically are dermal-based lesions with a peripheral zone that resembles a neurofibroma by virtue of the interdigitation of slender pigmented dendritic cells with surrounding collagen. The cells lack atypia and have small, pinpoint nucleoli (Fig. 30-42). Recurrent cellular blue nevi, however, can acquire more atypical cytologic features such that a distinction from clear cell sarcoma is not always possible. In these situations review of the original material and/or molecular genetic analysis is essential. The recently described paraganglioma-like dermal melanocytic tumor (PDMT), while having cells with a clear to eosinophilic cytoplasm, comprises zellballen-like nests of cells of distinctly low nuclear grade (Fig. 30-46A,B). These lesions, based in the dermis, rarely extend to deep structures. All thus far have behaved in a benign fashion.[126]
发生在浅表皮肤位置的病变不一定就是痣或恶黑,似乎不能轻易排除透明细胞肉瘤,好发于深部的CCS在皮肤发生也有报道,这无疑增加了诊断的难度:
Cutaneous Clear Cell Sarcoma: A Clinicopathologic, Immunohistochemical, and Molecular Analysis of 12 Cases Emphasizing its Distinction from Dermal Melanoma
Hantschke, Markus MD*; Mentzel, Thomas MD*; Rütten, Arno MD*; Palmedo, Gabriele PhD*; Calonje, Eduardo MD†; Lazar, Alexander J. MD‡; Kutzner, Heinz MD*
Clear cell sarcoma (CCS) of tendons and aponeuroses/malignant melanoma (MM) of soft parts is a rare tumor and in the majority of cases presents a characteristic reciprocal translocation t(12;22)(q13;q12) that results in fusion of the EWS and ATF1 genes. Although the melanocytic differentiation of CCS is indisputable, its precise lineage remains unclear. Typically, the slowly growing tumor affects the extremities of adolescents or young adults, especially around the ankle and foot. CCS is classically regarded as a deep soft tissue tumor associated with tendons or aponeuroses. This traditional view is put into perspective by the description of primary CCS of the gastrointestinal tract that may have a variant fusion gene EWSR1-CREB1. We describe 12 cases of cutaneous CCS and discuss the differential diagnoses. These 12 cases share an identical immunohistochemical profile with MM and thus can easily be confused with a dermal variant of spindle cell MM or metastasis of MM. The patients' ages ranged from 6 to 74 years (median: 25 y), and there was a female predominance (10 females, 2 males). Most tumors (n=9) were located on the extremities, 2 tumors arose on the back, and 1 on the abdomen. The mean tumor size was 0.97 cm (range, 0.4 to 1.7 cm). Six cases showed invasion of the subcutis, the other 6 cases were entirely dermal. Tumor necrosis was evident in 2 cases, melanin pigment in 2 cases, and ulceration in 1 tumor. All cases showed uniform nests and fascicles of pale spindled or slightly epitheloid cells with finely granular eosinophilic or clear cytoplasm. There was fair pleomorphism with plump spindled nuclei and significantly prominent nucleoli. Multinucleated wreath-like tumor giant cells were observed in two-thirds of cases, but were usually present only focally. The dense cellular aggregates were encased by delicate fibrous septa. The stroma showed a sclerotic reticulated pattern. Partly, the nests of spindle cells bordered the epidermis, prima vista mimicking junctional nests of melanocytes. The specific translocation pattern was confirmed in all cases by fluorescence in situ hybridization. Local recurrences and metastases developed in 2 and 3 patients, respectively, and 1 patient died of the disease.