| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 颞顶部占位:胶质瘤?增生?
-
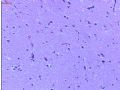
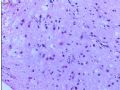
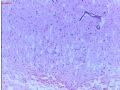
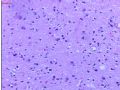
This is not an easy case to interpret. There is edema and gliosis in the brain parenchyma shown. Is the large structure in Figure 8 a large hyperchromatic nucleus? Figure 10 shows a few cells with possible cytologic atypia. Without hypercellularity, the significance of these rare atypical cells is difficult to determine. When in doubt, do immunohistochemical stains of MIB-1 (Ki67) and p53 for additional help.

聞道有先後,術業有專攻
如果活检标本太少,诊断病理医师要考虑标本能否代表核磁所反映的全部病变。再看一看核磁上肿瘤大小,形状,解剖部位,是否多灶性,病变的质地,周围有无水肿,对比增强改变。这些改变放射科医生诊断了什么?如果核磁考虑是高度恶性肿瘤或胶母细胞瘤,本例表现出的类似WHO分类的星形细胞瘤II 级或弥漫浸润性的星形细胞瘤诊断可能是错的。这是因为外科医生取活检的部位是肿瘤之边缘,并非中心,也不是分级最恶性的代表区域。
-
The immunostains clearly show many cells with strong nuclear immunoreactivity to antibodies against p53 and MIB-1 (Ki-67). These findings are diagnostic of an infiltrating fibrillary astrocytoma with low cellularity and, to the best I can tell from the photos, no readily identified mitoses. I am somewhat surprised to see so many positively stained cells in such low cellularity. This warns me to consider whether this is the edge of a high grade astrocytoma. The infiltrative borders of a high grade astrocytoma may look identical to the center of a WHO grade II astrocytoma. Therefore, grading of this tumor presented can be very tricky and depends on (1) how much tissue you have received for pathologic examination, and (2) pre- and post-surgical MRI findings. This needs to be carefully considered to avoid under-grading of a high grade astrocytoma.
If the specimen is from a stereotactic biopsy and small in amount, the interpreting pathologist has to try to determine whether the specimen represents the entire lesion found on MRI. The size, shape, anatomic location, multicentricity, heterogeneity of signal intensity, surrounding edema, and contrast enhancement on MRI are what radiologists look for in brain tumors. If MRI findings are consistent with a high grade tumor or glioblastoma, it would be wrong to grade this case as a WHO grade II fibrillary or diffuse infiltrating astrocytoma. This may happen when the surgeon biopsied the edge and not the center or worst area of the lesion.
From the gross description of this case, the specimen is probably from an open biopsy or subtotal resection. Sometimes, what we receive in the lab is not what the surgeons resect in the OR. A common scenario is that neurosurgeons send some tissue to pathology (with or without FS consultation request) they consider representative by their gross inspection. They will then continue to resect what they perceive as abnormal tissue, often with the help of CUSA (Cavitron Ultrasound Aspirator) that sucks soft abnormal tissue into a collector. These aspirated abnormal and normal tissue is admixed with foamy saline and blood, and often is difficult to harvest for adequate microscopic evaluation due to distortion. Some neurosurgeons don't even send this specimen to pathology and just discard it. In that case, what we receive in the lab is actually only a part of what surgeons resect. For these reasons, I almost always look at pre- and post-surgical MRI and read the operative note myself to be sure of the type of surgery (small biopsy vs resection), the pre-surgical MRI impression, and where the biopsy was on the post-surgical MRI. Only with this exercise would I be confident in diagnosing a WHO grade II diffuse infiltrating astrocytoma. After all, grade II astrocytomas are much less common than WHO grade IV glioblastomas in middle aged or elderly patients.

聞道有先後,術業有專攻
| 以下是引用mjma 在2006-11-18 0:09:00的发言: The immunostains clearly show many cells with strong nuclear immunoreactivity to antibodies against p53 and MIB-1 (Ki-67). These findings are diagnostic of an infiltrating fibrillary astrocytoma with low cellularity and, to the best I can tell from the photos, no readily identified mitoses. I am somewhat surprised to see so many positively stained cells in such low cellularity. This warns me to consider whether this is the edge of a high grade astrocytoma. The infiltrative borders of a high grade astrocytoma may look identical to the center of a WHO grade II astrocytoma. Therefore, grading of this tumor presented can be very tricky and depends on (1) how much tissue you have received for pathologic examination, and (2) pre- and post-surgical MRI findings. This needs to be carefully considered to avoid under-grading of a high grade astrocytoma. |
I agree with Dr. Ma's comment, this tissue dose like so called "CUSA" tissue, Some US pathologist rrefuses to read those cases. please show us some more photos if you have, otherwise, you may need to talk to your neurosurgeons. As a pathologist, educttion is a lifelong duty, sorry.