| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 反复肠梗阻剖腹探查
| 姓 名: | ××× | 性别: | 男 | 年龄: | 79 |
| 标本名称: | 回盲部 | ||||
| 简要病史: | 老年男性,79岁。因"反复腹痛、腹胀4月,再发3天"入院 | ||||
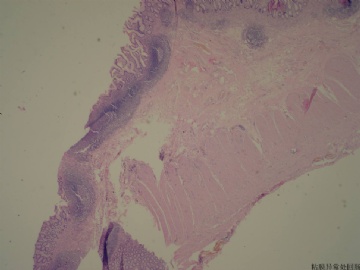
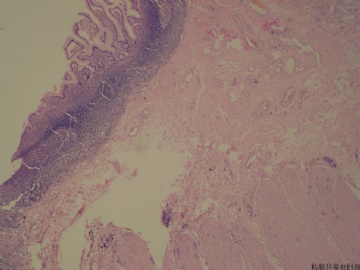
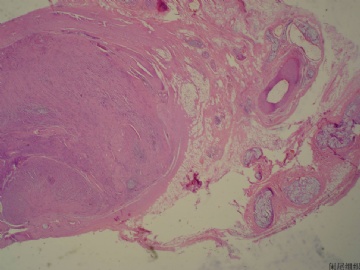
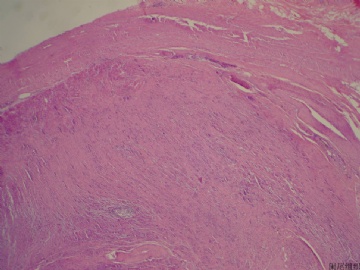
| 肉眼检查: | 大体检查:回盲肠一段,回肠长约19cm,盲肠长约10cm,回肠明显扩张直径4.8cm,切面见回盲瓣处明显狭窄,粘膜面未见异常,近回盲瓣处回肠局部粘膜约11X1.5cm的区域粗糙(呈矩形分布),粘膜呈粗颗粒状,此处病变回肠切面未见肿块。阑尾长约2cm,最大直径0.9cm,呈实性变,质脆。升结肠残端未见明确异常。 其它: 查体:腹平坦,未见明显胃肠型及异常蠕动波,叩诊鼓音,全腹软,左侧腹压痛,无明显反跳痛及肌紧张;未扪及异常包块,移动性浊音阴性,肠鸣音活跃,约6次/分,未闻及汽过水声 | ||||
-
本帖最后由 于 2011-03-23 21:59:00 编辑
PDF复制下来的排版不好看,见谅
GOBLET CELL CARCINOIDS OF THE APPENDIX
Goblet cell carcinoids (GCCs; synonymous terms:
adenocarcinoids, goblet cell tumors) have mixed pheno-
types, with partial neuroendocrine differentiation and
intestinal goblet cell morphology. Goblet cell carcinoids
are classified as mixed endocrine-exocrine tumors; they
are considered to represent a separate clinicopathologic
entity, distinct from both classic AET and appendiceal
adenocarcinomas, but their histogenesis is unclear. They
have amore aggressive history than classic AET and, thus,
require a different diagnostic and therapeutic ap-
proach.
1,28–31
Epidemiology and Symptoms
The incidence of GCC is estimated to be one-tenth of
that for AETs. In contrast to classic AET, roughly equal
numbers of men and women develop GCC.Median age at
presentation is later than for AET, during the fifth decade,
with a second peak at 70 years.
5,6,31–33
Goblet cell carcinoids
usually manifest as abdominal pain and a palpable mass
(in patients with advanced disease) or acute appendicitis.
Concomitant metastases (mostly ovaries, right colon, and
peritoneum) are present at diagnosis in more than half of
the patients.
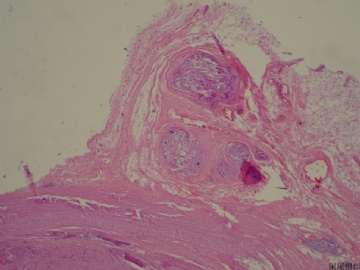
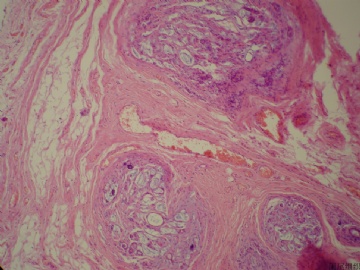
Location and Size
Goblet cell carcinoids are usually located in the middle
third of the appendix and may well cause longitudinal
extension and appendiceal obstruction. They usually lack
the formation of a well-defined tumor mass; thus, it is
somewhat difficult to accurately assess their size. How-
ever, a recent study showed that most GCCs are larger
than 2 cm in size.
29
Size correlates with survival when
analyzed by the following cutoff points: smaller than 1 cm,
between 1 and 2 cm, and larger than 2 cm.
32
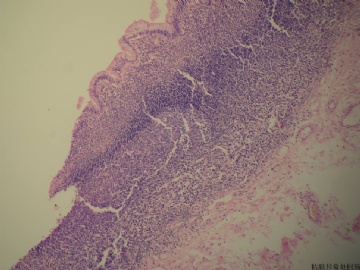
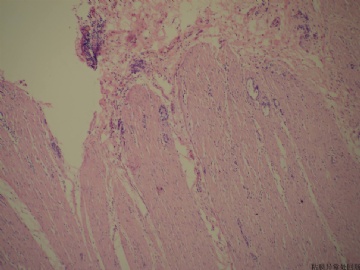
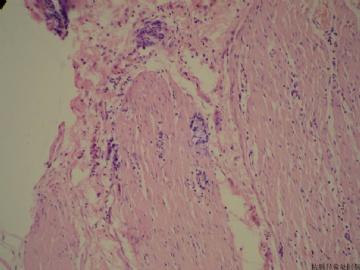
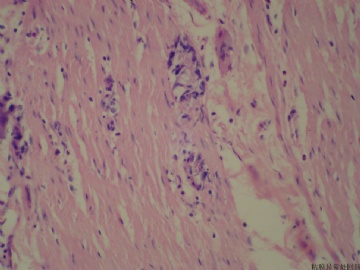
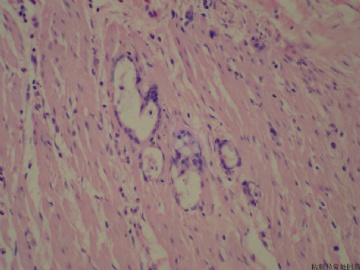
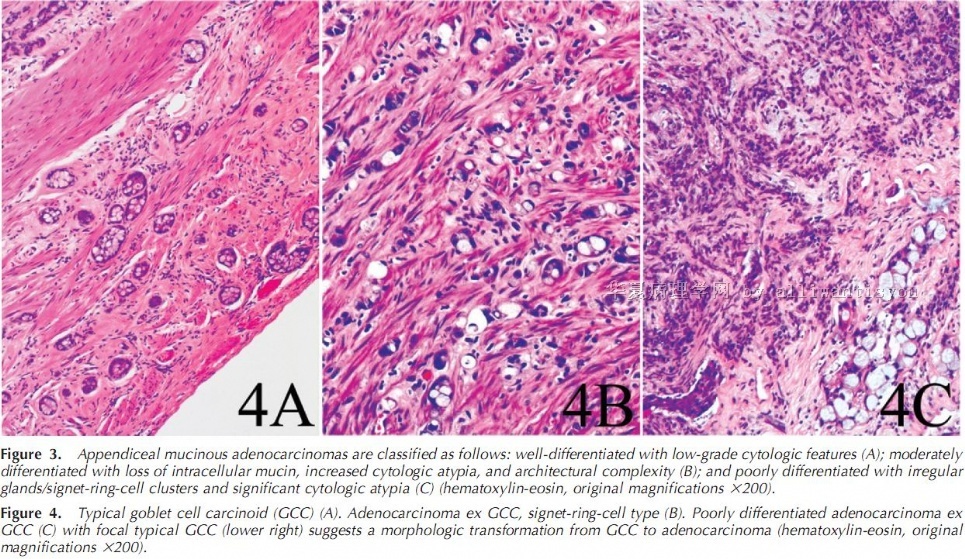
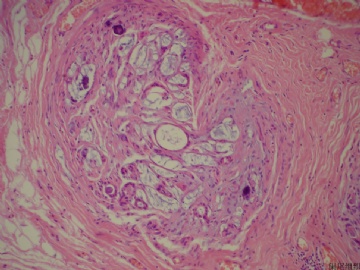
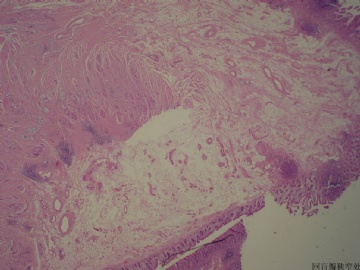
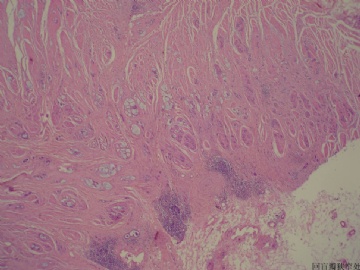
Histopathologic Diagnosis of GCC
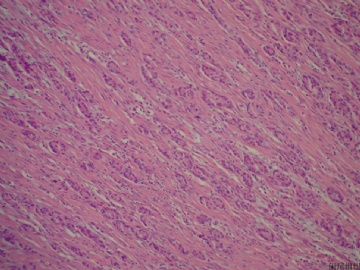
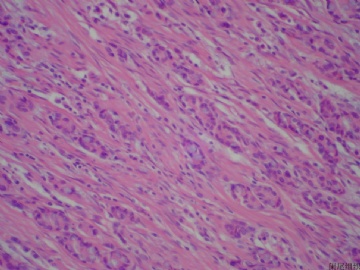
Histology.—Typical GCCs have a mixed phenotype,
with partial neuroendocrine differentiation and intestinal-
type goblet cell morphology. Indeed, they are character-
ized by the presence of mucin-containing, goblet-shaped
epithelial cells, arranged in round or oval clusters
(Figure 2, a and b). Mucin stains (periodic acid–Schiff,
periodic acid–Schiff diastase, Alcian blue) are strongly
positive within goblet cells (Figure 2, c) and may
underline the presence of pools of extracellular mucin.
The cells exhibit minimal cytology atypia, and there are
rare or no desmoplastic stroma (Figure 2, b). The clusters
are oriented along the axis of the muscle fibers of the
muscularis propria (Figure 2, d); they characteristically
spare the mucosa.
29
A recent retrospective study29
of a
large number of GCC cases (n 5 63) has shown that the
cases could be stratified into 3 morphologic groups: (1)
typical GCC, as described above; (2) adenocarcinomas,
signet ring cell type; and (3) adenocarcinomas, poorly
differentiated. The last 2 groups contain at least a focal
component typical of GCC. Interestingly, this classifica-
tion correlates with patient survival.
29,34
The authors29
suggest that GCCs display a spectrum of histologic
features and possess the potential to progress to an
aggressive adenocarcinomas phenotype.
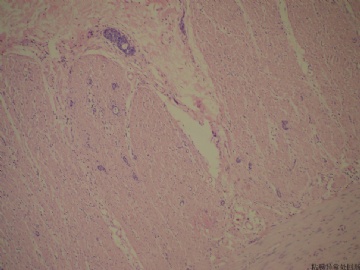
Immunohistochemistry.—Immunohistochemistry with
chromogranin A and synaptophysin antibodies demon-
strate focal reactivity (in 5%–25% of tumor cells), in
contrast to the diffuse staining in most classic AETs
(Figure 2, d). MUC2 staining results are positive in GCCs,
and the CK7/CK20 profile is different from classic
AET.
Other immunohistochemical markers for ma-
lignant behavior, such as b-catenin, E-cadherin, p53, or
CK19, are not required on a routine basis because their
prognostic value has not been validated in GCC.
21,35–37
In
addition, molecular analysis of GCC has shown a
significant overlap with classic AET.
38
Proliferation Rate.—Mitotic figures are rarely identified
in GCC. Some data include the proliferation marker Ki-67
or the number of mitoses as prognostic indicators in
GCC.
20,39
In a recent study, Tang et al
29
found a
proliferative index at 11% (SD 5 2%) in a large series of
GCC.
29
Mitotic index and Ki-67 should probably be
assessed, following the consensus recommendations of
the TNM for digestive endocrine tumors, but their
correlation with prognosis is unclear in GCCs.
23
Tumor Infiltration.—Appendiceal Wall Infiltration.—Sero-
sal involvement, invasion of the mesoappendix, or
extension into the peritoneum or adjacent organs are
prognostic factors in GCC. Mesoappendiceal involvement
is frequent and was observed in 51% of cases in a recent
series of 227 patients39
; lymph node metastases are
detected in 34% of patients with GCC, and the pattern of
extension is predominately limited to the pelvic organs
with peritoneal spread.
Surgical Margins.—The surgical margins (R0/R1) must
be reported clearly. However, the diagnosis of GCC
generally leads to a right hemicolectomy (see discussion
below), even when the appendiceal margin is negative for
cancer cells.
Classifications.—Goblet cell carcinoids are classified
according to the WHO and to TNM staging:
WHO Classification.—In the last version of the WHO
classification for endocrine tumors (Table), GCCs were
classified as mixed exocrine-endocrine carcinoma along
with other, low-grade, malignant tumors.
TNM Classification.—The TNM classification and grading scheme proposed for digestive endocrine tumors and used for classic AETs should not be used for GCCs. The preferred TNM classification is the one used for appendiceal adenocarcinomas.
Prognosis and Guidelines for Follow-up and Surgical Therapy Goblet cell carcinoids bear a worse prognosis than classic AET (GCC 5-year survival rate, 76%; AET 5-year survival rate when all stages are included, 83%). Right hemicolectomy, to be performed after initial appendectomy, is considered the standard surgical intervention for GCC.This implies that the diagnosis of GCC on frozen section examination leads to a right hemicolectomy.However, some authors have shown that low-risk tumors (,1 cm; localized; without serosal, mesoappendiceal, or cecal invasion; with low proliferative index) can be better served with appendectomy alone.Cytoreductive surgery with adjuvant chemotherapy or intraperitoneal chemotherapy may prolong survival in cases with advanced peritoneal dissemination.
World Health Organization Classification of Endocrine
Tumors of the Appendix
A. Well-differentiated endocrine tumor
1. Benign behavior
N Nonfunctioning, and
N Confined to appendiceal wall, and
N #2 cm, and
N Nonangioinvasive, and
N Ki-67 index of #2%, and
N Mitoses of #2 cells/high-power fields 340
2. Uncertain behavior
N Nonfunctioning, and
N Confined to subserosa, or
N .2 cm, or
N Angioinvasive
B. Well-differentiated endocrine carcinoma, low-grade,
malignant
N Invading the mesoappendix or beyond, and/or
N With metastases,
N With or without a functioning (carcinoid) syndrome
C. Mixed exocrine-endocrine carcinoma
1. Low-grade, malignant, goblet cell carcinoids
Data derived from Solcia et al.