| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
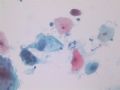
- 花季少女,如何下诊断?
-
本帖最后由 于 2007-11-03 21:53:00 编辑
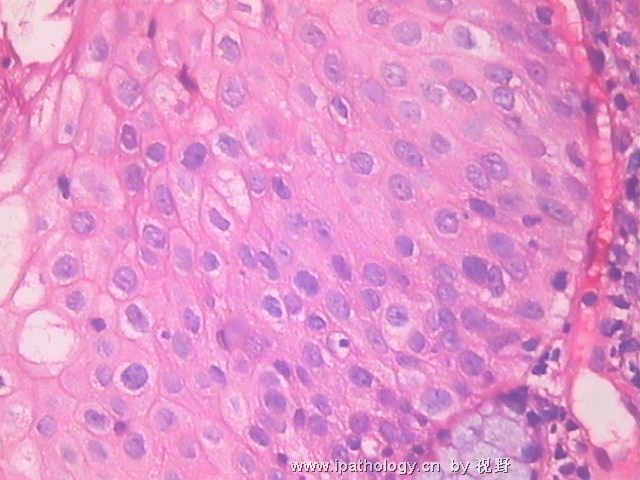
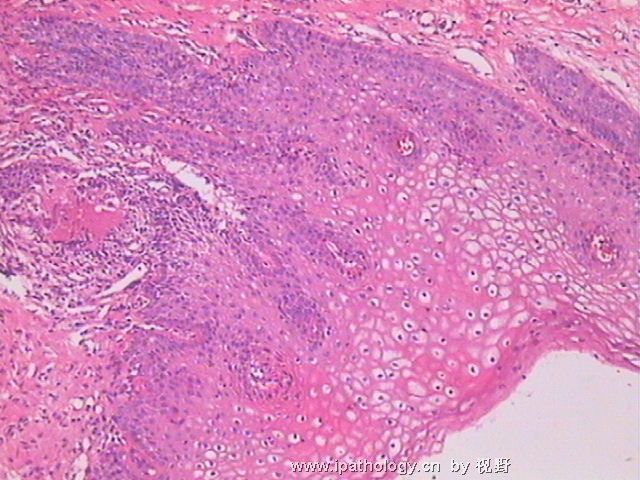
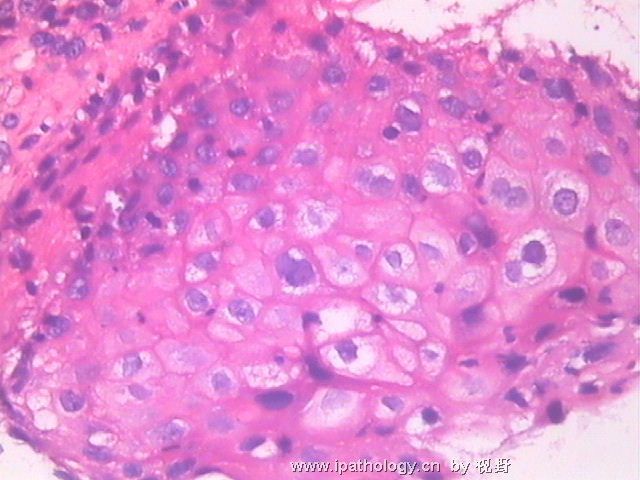
I agree with all your concern for HSIL in this case. However, I will be cautious for that diagnosis given her age of 19. As cervical smear is a screening test, not final diagnosis, you need to carefully think what your diagnosis will trigger the next step of clinical management. She has obviously LSIL in first few slides and couple groups of cells with increased N/C ratio concerning for HSIL. In our hospital, we have a diagnosistic category of " LSIL, cannot rule out HSIL" . It will trigger the biopsy in clinical management, but leave little space for yourself. I will render the diagnosis of " LSIL, cannot rule out HSIL" in this patient.
If you are doing both cytology and gynecologic surgical pathology, you will know we have overdiagnosed lot of the cases. Please think about this, if you make straight forward diagnosis of HSIL and follow up biopsy is just LSIL, you will force the clinician to do more. In US, as the malpractice insurance for OB/GYN clinicians is so high, based on you non-hesitating diagnosis of HSIL, GYN clinian will do LEEP if biopsy of this cytologically HSIL turns out to be negative for CIN2+, because they realy worry they may miss the HSIL on biopsy since the accuracy to pick up CIN2+ lesions by colposcopic-directed biopsy is only about 57% for colposcopic experts in US. For this patient, I would like to alert the GYN clinician to closely follow the patient up, but not overdo it to cause harm to the patient. To me, PAP diagnosis is not just based on the "cytomorphology". You have to constantly think what the clinical management you diagnosis will imply or trigger, as we are not just "diagnosticians" or "slide readers" but the part of the patient care team.
That is not to say there is no HSIL in this young age. I have seen HSIL and CIN2+ at age of 15. However, you have to keep in mind that epidemiologically most HPV infections before age 25 are transient, not persistent, and up to 90% of LSIL and up to 60% of CIN2 will regress on its own. If the similar smears for a 35 year old patient, I may go all the way to HSIL since in that age group, persistent HPV infection and CIN2+ lesions are much higher than those below 20. Thereforre, understanding the clinical situation is one of the most important factors in making pathologic diagnostic desicion.
(我同意大家担心此例为HSIL。然而,19岁的年龄,我会非常谨慎地使用这个诊断。由于宫颈涂片只是筛查检测,不是最终诊断,因此需要考虑到你们的诊断会引发什么后续的临床处理。图片中有明显的LSIL,并有几团细胞核/浆比增加使人担心HSIL。我们医院有一个诊断分类为“LSIL但不能除外HSIL”。它会引发活检这一临床处理,但给你们留下的空间很少。此例我会使用“LSIL但不能除外HSIL”这一诊断。
如果你们同时做细胞学和妇科病理,你会发现我们有很多过诊断病例。请考虑这一点,如果直接诊断了HSIL但随访活检只是LSIL,你会给临床医生添麻烦。在美国,妇产科医生的医疗事故保险很高,是基于你们毫不犹豫的诊断HISL。如果细胞学HSIL在活检时变成未见CIN2+,妇科医生仍会做LEEP手术,因为他们担心活检时可能漏掉HSIL---在美国阴道镜专家检出CIN2+病变的活检准确率只有57%。对本例,我会警告妇科医生密切随访,但不能过度处理(治疗)而导致对患者的损伤。对我来说,PAP诊断并非仅根据“细胞形态学”。你们必须时刻考虑诊断意味着或会引发何种临床处理,因为我们不只是“诊断师”或“读片匠”,而是治疗团队的一部分。
但这并不是说这样年轻就没有HSIL。我曾见过15岁的HSIL和CIN2+。然而必须牢记,流行病学上,绝大多数25岁以前的HPV感染都是一过性的,不是持续性的,90%的LSIL和高达60%的CIN2会自发消退。如果35岁患者出现相似的表现,我会直接报HSIL因为这个年龄组的持续HPV感染和CIN2+病变比20岁以下者的发病率高得多。因此,在做出病理诊断时,理解临床情形是最重要的因素之一。 --abin译)

- 不坠青云之志,长怀赤子之心