| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
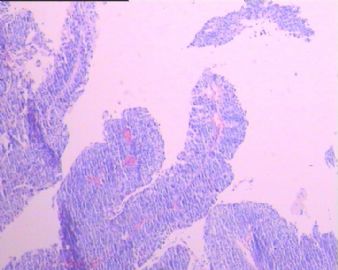
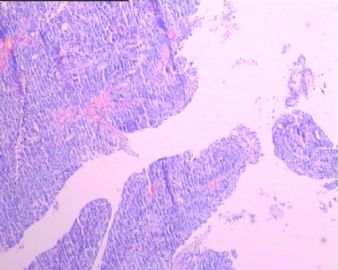
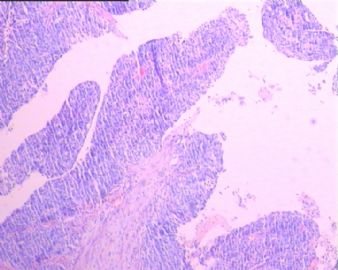
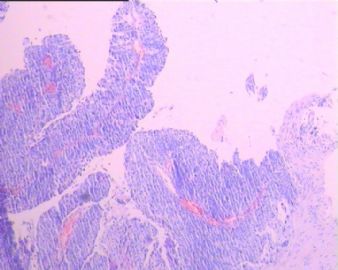
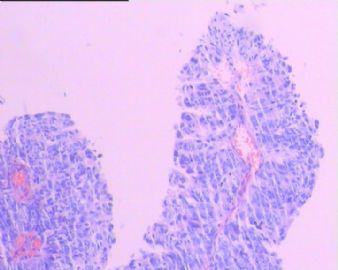
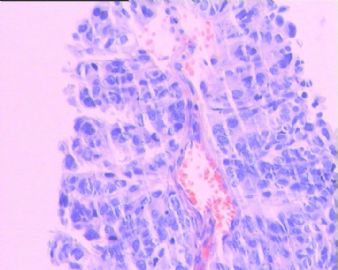
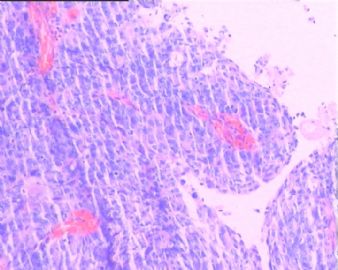
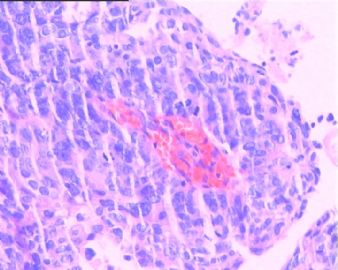
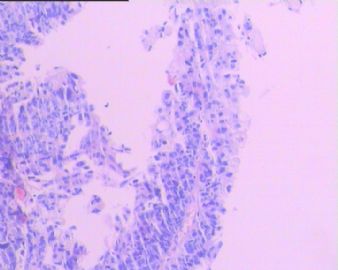
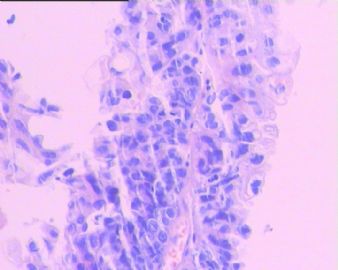
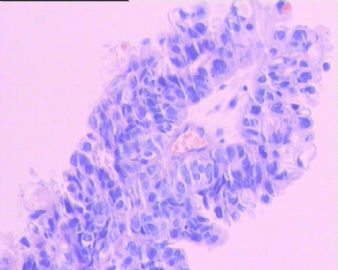
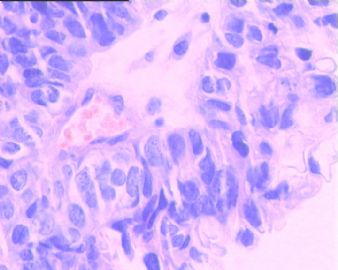
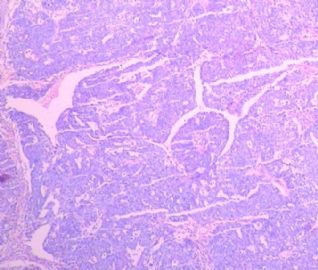
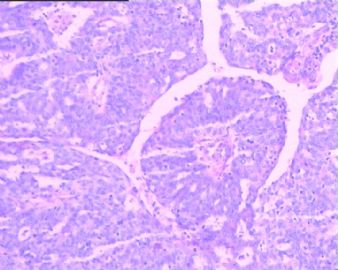
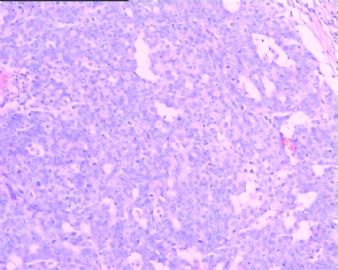
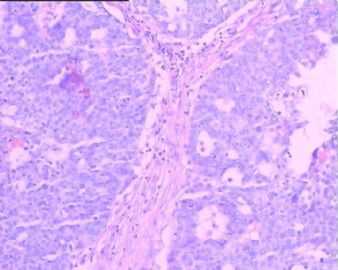
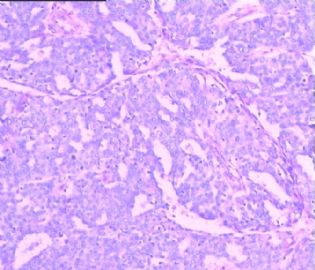
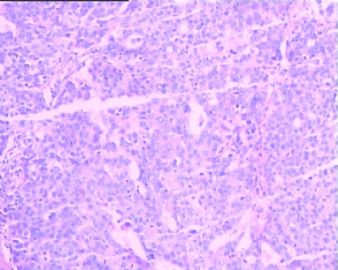
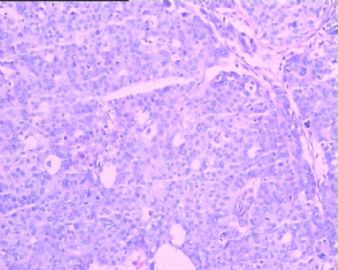
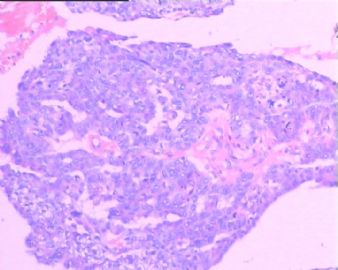
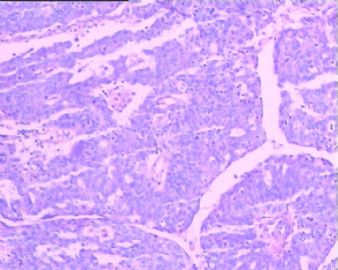
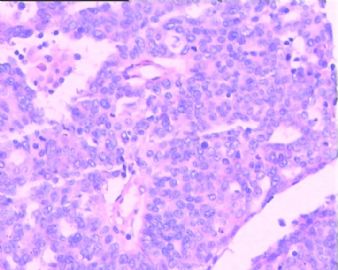
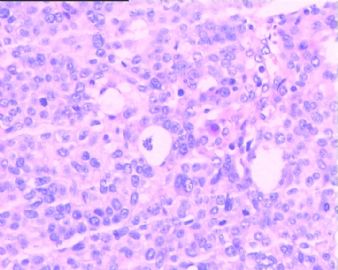
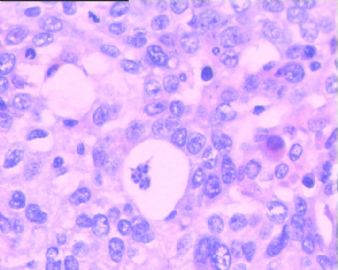
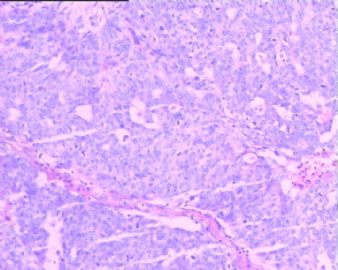
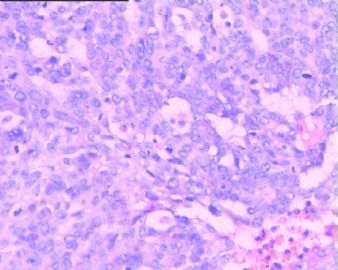
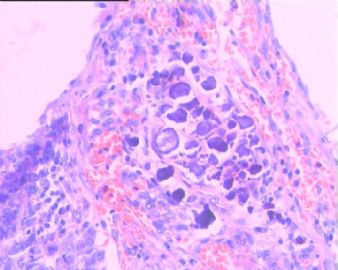
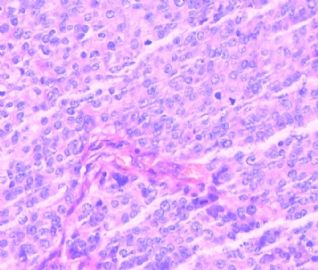
- 卵巢癌病理类型?
| 姓 名: | ××× | 性别: | 女 | 年龄: | 47 |
| 标本名称: | |||||
| 简要病史: | |||||
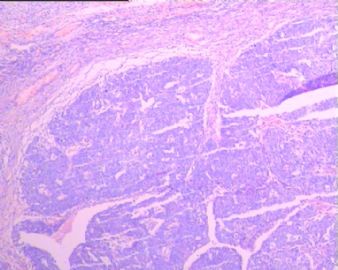
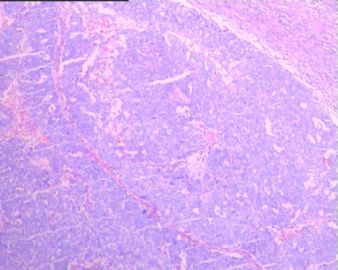
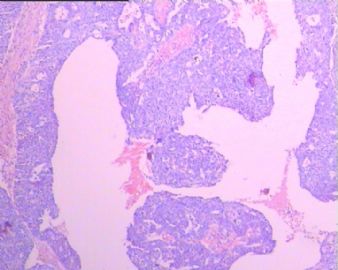
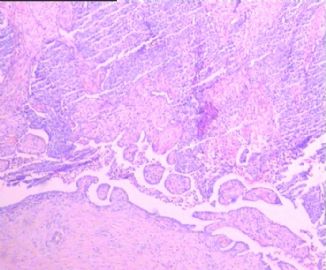
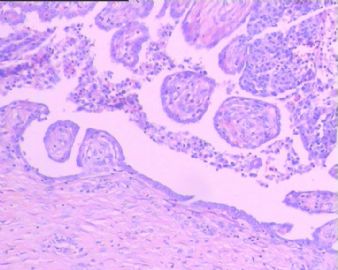
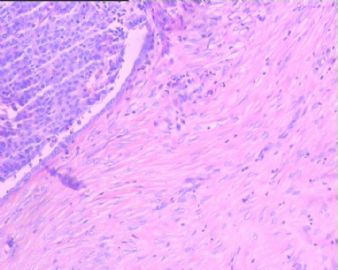
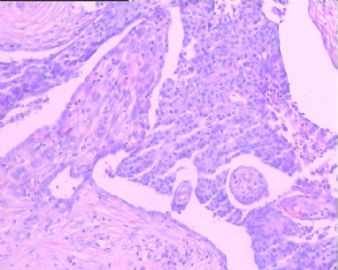
| 肉眼检查: | 左卵巢囊性肿瘤8*6*5厘米,内壁弥漫性乳头状突起,最大的直径1.0厘米,花菜样,切面见囊壁浸润。左输卵管腔内少许花菜样肿瘤组织。 | ||||
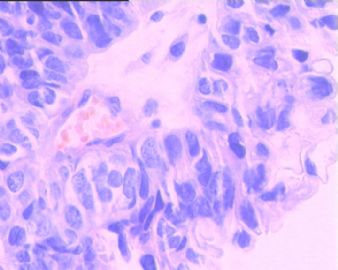
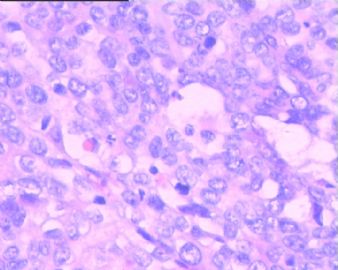
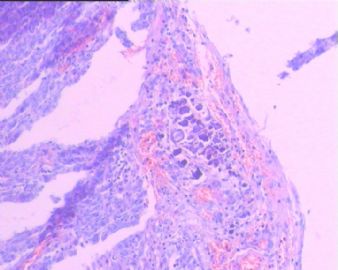
镜下检查:部分乳头状区,部分实性区内有腺样结构,灶性钙化。
免疫组化:选实性区标记 ck7+ ck20- p53+ p63-
-
本帖最后由 于 2010-09-27 17:25:00 编辑
低分化的浆乳癌与移行细胞癌常常带给我们鉴别诊断的难题,本例即如此。下面这篇文献或许可供参考。Am J Surg Pathol. 2004 Apr;28(4):453-63.Transitional cell carcinoma of the ovary: a morphologic study of 100 cases with emphasis on differential diagnosis.Eichhorn JH, Young RH.
Abstract
Transitional cell carcinoma (TCC) of the ovary is a recently recognized subtype of ovarian surface epithelial-stromal cancer, and studies of its morphology are few. As a result, the criteria for its diagnosis and spectrum of its morphology are not clearly established. One hundred consecutive consultation cases of ovarian carcinoma with a pure or partial transitional cell pattern (excluding malignant Brenner tumor) diagnosed between 1989 and 2001 were evaluated for the frequency of various pathologic features and the relation of TCC to other surface epithelial-stromal carcinomas. The women were 33 to 94 years of age (mean, 56 years). A total of 47 tumors were stage I, 21 stage II, 31 stage III, and 1 stage IV; 13% of the stage I tumors and 41% of tumors of all stages were bilateral. The tumors ranged from 3.0 to 30 cm in greatest dimension (mean, 10 cm); 60% of them were solid and cystic, 24% solid, and 16% cystic. TCC was the exclusive or predominant component in 93% of the tumors and showed undulating (93%), diffuse (57%), insular (55%), and trabecular (43%) patterns. In four tumors with an insular growth, the pattern focally mimicked a Brenner tumor. Necrosis was present in 57% of the cases. Features that were seen in the tumors that in aggregate produced a relatively consistent appearance were "punched out" microspaces (87%), often the size of Call-Exner bodies, large cystic spaces (73%), and large blunt papillae (63%). Features that were sometimes seen, usually as a focal finding, included slit-like fenestrations (49%), bizarre giant cells (35%), small filiform papillae (18%), gland-like tubules (17%), squamous differentiation (13%), and psammoma bodies (4%). In 23 cases, TCC was a component of a mixed epithelial carcinoma, the additional components being serous adenocarcinoma in 16, endometrioid in 5, mucinous in 1, and clear cell carcinoma in 1. The tumor cells of the TCC component often were relatively monomorphic; 6% of the tumors were grade 1, 43% grade 2, and 51% grade 3. The nuclei were oblong or round and often had large single nucleoli (69%) or longitudinal grooves (48%). The cytoplasm was typically pale and granular but was rarely strikingly clear or oxyphilic. TCC of the ovary usually occurs in pure form but is also common as a component of a surface epithelial carcinoma of mixed cell type. In either situation, TCC has a constellation of architectural and cytologic features that readily distinguish it in most cases from other types of ovarian cancer. Recognition of these features will lead to a more consistent diagnosis of this tumor and aid in determining whether it has distinctive clinical features, particularly with regard to its behavior.

- If you have great talents, industry will improve them; if you have but moderate abilities, industry will supply their deficiency. 如果你很有天赋,勤勉会使其更加完美;如果你能力一般,勤勉会补足其缺陷。
Clearly there are a lot of areas showing classic papillary serous ca. It is true foci show transitional-like pattern. See carefully and you will notice that they are large papillary structure.
In addition, pur high grade papillary ca and high grade papillary serous ca mixed with transtional ca will not show difference in term of treatment and prognosis.
I will sign out the case as high grade seous ca and read next case.
-
hanxinliang 离线
- 帖子:46
- 粉蓝豆:1
- 经验:261
- 注册时间:2008-01-07
- 加关注 | 发消息
| 以下是引用天山望月在2010-9-28 22:46:00的发言:
移形细胞癌P63标记阳性,此例标记阴性,不知是否能解释?谢谢! |

- 王军臣