| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 移植肾穿刺病例
-
本帖最后由 于 2010-09-16 21:08:00 编辑
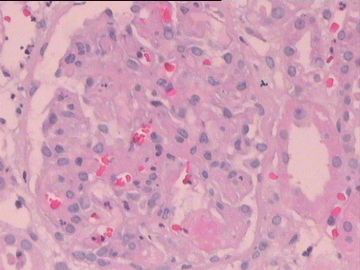
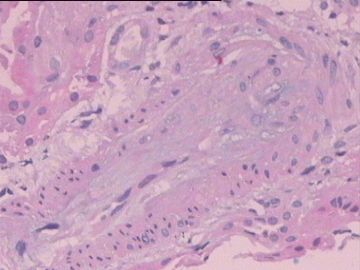
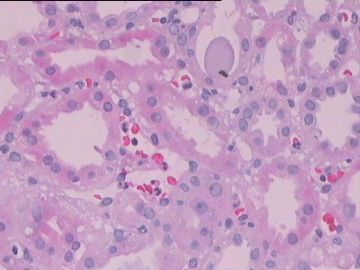
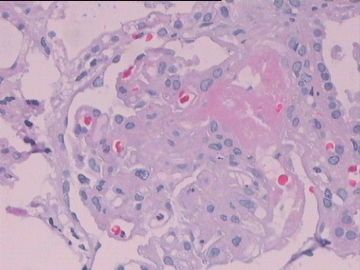
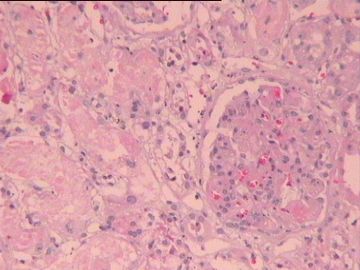
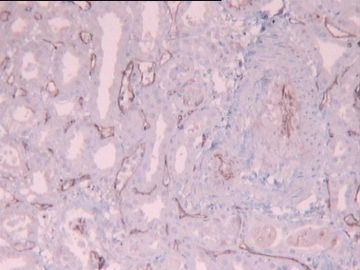
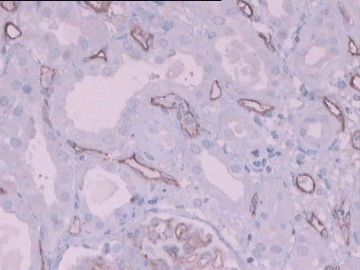
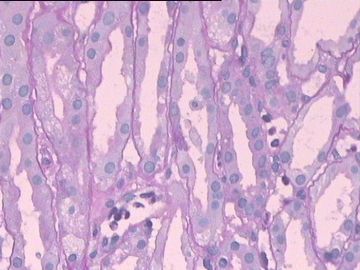
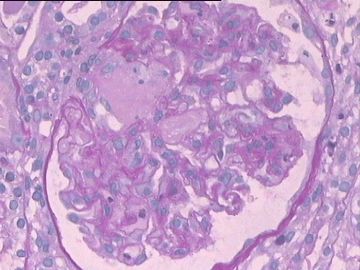
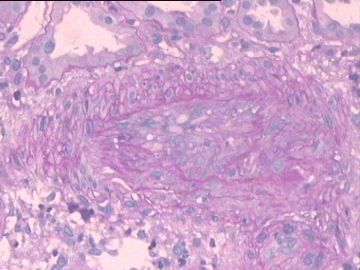
Fig. 1, 4, 5 and 9 show microthrombi in glomerular capillaries. Given the positive C4d stain, acute antibody-mediated rejection is suggested. Drug induced HUS is the differential diagnosis. But the C4d result and patchy tubular necrosis in Fig. 5 favor acute antibody-mediated rejection. The arteries demonstrate intimal edematous change. My experience tells me that the edematous change is non-specific.
-
hailuonvhai 离线
- 帖子:4
- 粉蓝豆:1
- 经验:59
- 注册时间:2010-09-14
- 加关注 | 发消息
肾移植术后血栓性微血管病(Thrombotic microangiopathy after kidney transplantation)。结合免疫组化C4阳性,符合为急性抗体介导的移植排斥反应。
参考文献:
The glomeruli show thrombosis or neutrophils or mononuclear leukocytes in capillary lumens. The tubulointerstitial compartment shows edema, hemorrhage, necrosis, mild inflammation, and neutrophils or mononuclear leukocytes in the peritubular capillary lumens. The blood vessels show thrombosis, thrombotic microangiopathy, fibrinoid necrosis, or transmural vasculitis. Strong staining for C4d in the peritubular capillaries is characteristic. A definitive diagnosis of AMR requires (1) morphologic evidence of acute tissue injury, (2) immunopathologic evidence for antibody action, and (3) serologic evidence of circulating donor-specific antibodies. Acute antibody-mediated rejection should be suspected if some but not all 3 criteria are met. -Arch Pathol Lab Med. 2007 Aug;131(8):1200-8.
In the literature, the most-frequent cause of hemolytic uremic syndrome in patients following renal transplantation is recurrence of the hemolytic uremic syndrome. Other causes include drug-related (cyclosporine, tacrolimus) toxicity, procoagulant status, and antibody-mediated rejection. We found that the most-frequent cause of thrombotic microangiopathy was drug related, secondary mainly to cyclosporine. -Exp Clin Transplant. 2004 Dec;2(2):268-72.