| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 子宫内膜
Eur J Gynaecol Oncol. 2010;31(2):160-4.
Expression and significance of beta-catenin, Glut-1 and PTEN in proliferative endometrium, endometrial intraepithelial neoplasia and endometrioid adenocarcinoma.
Department of Gynecological Oncology, Zhongnan Hospital, Wuhan University, Wuhan, China. ybeary@hotmail.com
Abstract
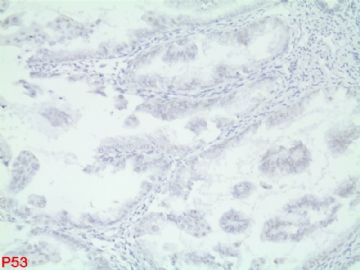
OBJECTIVE: The aim of this study was to explore the potentiality of beta-catenin, Glut-1 and PTEN proteins as markers for a diagnosis of endometrial intraepithelial neoplasia (EIN). DESIGN: Ten proliferative endometrium, 83 endometrial hyperplasia (59 benign hyperplasia, 24 EIN) and 24 endometrioid adenocarcinoma sections were immunostained for beta-catenin, Glut-1 and PTEN protein expression. RESULTS: (1) Abnormal expression of beta-catenin was detected in 10% of benign hyperplasia, 50% of EIN and 67% of endometriold adenocarcinoma. (2) Overexpression of Glut-1 was present in 58% of EIN and 71% of endometrioid adenocarcinoma. (3) Complete loss of PTEN immunoreactivity was found in 20% of proliferative endometrium, 29% of benign hyperplasia, 38% of EIN and 63% of endometrioid adenocarcinoma. CONCLUSIONS: The abnormal expression of beta-catenin and overexpression of Glut-1 may be useful markers in distinguishing benign hyperplasia from EIN, whereas lack of PTEN expression is not an appropriate marker for a diagnosis of EIN.
Diagn Pathol. 2009 Nov 25;4:41.
Altered PTEN expression; a diagnostic marker for differentiating normal, hyperplastic and neoplastic endometrium.
Sarmadi S, Izadi-Mood N, Sotoudeh K, Tavangar SM.
Department of Pathology, Mirza Koochak Khan Hospital, Tehran University of Medical Sciences, Tehran, Iran. ssarmadi@yahoo.com
Abstract
BACKGROUND: Different molecular alterations have been described in endometrioid endometrial carcinoma (EECA). Among them the most frequently altered is loss of the PTEN protein, a tumor suppressor gene. The purpose of this study was to evaluate the expression pattern of PTEN gene in normal, hyperplastic and neoplastic endometrium. METHODS: In a study in a referral gynecologic hospital in Tehran, Iran, immunohistochemical (IHC) evaluation of PTEN was performed on 87 consecutive specimens to the following three groups; group A- normal proliferative endometrium(n = 29); group B- hyperplastic endometrium [including simple hyperplasia without atypia(n = 21) and complex hyperplasia with atypia (n = 8)] and group C- EECA(n = 29). Immunostaining of cells was analyzed by arbitrary quantitative methods according to both slide's area staining and intensity of color reaction. RESULTS: PTEN immunoreactivity was present in all normal proliferative endometrium, all simple hyperplasia, 75% of atypical complex hyperplasia and in 48% of EECA (P < 0.001). The intensity of PTEN reaction was significantly higher in group with proliferative endometrium than hyperplastic endometrium and EECA (P < 0.001). CONCLUSION: PTEN expression was significantly higher in cyclical endometrium than in atypical hyperplasia and endometrioid carcinoma.
PMID: 19930726 [PubMed]PMCID: PMC2789036Free PMC Article

- 王军臣
-
3.
Int J Gynecol Pathol. 2009 Sep;28(5):471-6.
Utility of PTEN expression of endometrial "surface epithelial changes" and underlying atypical endometrial hyperplasia.
Quddus MR, Ologun BA, Sung CJ, Steinhoff MM, Lawrence WD.
Department of Pathology, Women & Infants Hospital, Providence, RI, USA. mquddus@wihri.org
Abstract
Surface epithelial changes (SECs) have been reported to be associated with endometrial carcinoma in about 49% of cases. They have also been seen to be associated with endometrial hyperplasia. Although morphologically benign, these lesions are considered a marker for underlying malignancy. Their true biologic nature, however, is not known. PTEN has been reported to be altered in endometrial carcinomas and endometrial precancers where no morphologic changes are appreciated. The current study aims to investigate PTEN status in the endometrial SECs. Thirty-two cases of endometrial biopsy are divided into 2 groups: group 1 had 18 cases of SEC and underlying endometrial atypical hyperplasia and group 2 had 14 cases of SEC alone. Four-micron sections were cut from each block and stained with antibodies to PTEN. One section was stained with hematoxylin and eosin to confirm the presence of the area of interest. Positive and negative control slides were run with each batch of staining. All 32 cases were followed for a median period of 54 (range, 21 to 84) months. Overall, PTEN alteration (NULL) was found in 12 of the 32 cases of endometrial samples (37.5%) examined. In group 1, 10 of the 18 cases (56%) of atypical endometrial hyperplasia with "SECs" showed PTEN NULL. Of these 10 cases, 6 (60%) cases showed FIGO grade 1 endometrioid carcinoma in subsequent hysterectomy specimens. Two other cases (20%) had atypical endometrial hyperplasia only. In group 2, two of the 14 (14%) cases of SECs alone showed PTEN NULL phenotype. These 2 patients were followed for 26 and 63 months, respectively, and subsequent endometrial biopsies and pap smears were negative. Of the remaining 12 cases that retained PTEN, 9 cases (75%) were negative when followed for a median of 54 months (range, 21 to 84 mo). SECs seem to be a heterogeneous entity. Presence of PTEN NULL phenotype in SECs and associated endometrial hyperplasia does not necessarily predict an increased incidence of endometrioid carcinoma in subsequent follow-up. However, absence of PTEN NULL phenotype in SECs alone may predict a benign follow-up.
PMID: 19696618 [PubMed - indexed for MEDLINE]
Pathol Res Pract. 2007;203(3):153-62. Epub 2007 Feb 20.
Immunohistochemical expression of PTEN in normal, hyperplastic and malignant endometrium and its correlation with hormone receptors, bcl-2, bax, and apoptotic index.
Kapucuoglu N, Aktepe F, Kaya H, Bircan S, Karahan N, Ciriş M.
Department of Pathology, Suleyman Demirel University, 32260 Cünür, Isparta, Turkey. kapucuoglun@gmail.com
Abstract
PTEN is a tumor suppressor gene that is frequently mutated in type I endometrioid endometrial carcinomas (EECs), and is involved in the control of cell proliferation, differentiation, and apoptosis. In this study, we aimed to assess the relationship between PTEN expression and estrogen, progesterone receptors (PRs), other apoptosis-related proteins, such as bcl-2 and bax, and apoptotic index (AI) in EEC, its precursor lesion hyperplasia, and cyclical endometrium. We also evaluated the relationship between PTEN expression and clinicopathologic parameters. PTEN, estrogen receptor (ER), PR, and bcl-2 and bax expressions were evaluated immunohistochemically, and AI was evaluated in hematoxylin and eosin (HE)-stained slides in 23 cyclical and 37 hyperplastic endometria and in 35 EECs. PTEN expression was higher in cyclical endometrium than in the carcinomas (p<0.05). The PTEN expression level was significantly higher in non-atypical hyperplasias than in EEC, but there were no differences between atypical complex hyperplasia (ACH) and EEC and between hyperplasias. In the carcinomas, there was a negative correlation between grade and PTEN expression (r=-0.338, p=0.047). In conclusion, we presume that PTEN is involved in the early phases of endometrial tumorigenesis, and it can be speculated that decreased PTEN expression with loss of differentiation in carcinoma can contribute to the emergence of tumors with a more aggressive phenotype.
PMID: 17317031 [PubMed - indexed for MEDLINE]
Int J Gynecol Cancer. 2006 May-Jun;16(3):1412-8.
Expression of survivin, PTEN and p27 in normal, hyperplastic, and carcinomatous endometrium.
Erkanli S, Kayaselcuk F, Kuscu E, Bagis T, Bolat F, Haberal A, Demirhan B.
Department of Obstetrics and Gynecology, Baskent University Faculty of Medicine, Seyhan, Adana 01250, Turkey. serkanli@tnn.net
Abstract
We aimed to investigate if expressions of survivin and p27 proteins are involved in the development of endometrioid carcinoma, along with whether there are any correlations between these proteins and loss of wild-type PTEN that is found in up to 80% of endometrial carcinomas. We also studied their correlations with classical prognostic factors and survival in endometrial carcinoma. To our knowledge, this is the first time survivin expression is investigated in endometrial hyperplasia along with endometrioid adenocarcinoma. For immunohistochemical analysis, 29 endometrioid adenocarcinoma, 38 endometrial hyperplasia, and 10 proliferative endometrium tissue samples were selected in the pathology archives. Staining of cells was scored as +2 if >50%, +1 if <50%, and negative if none were stained positive. Survivin expression increased from proliferative to hyperplasia to carcinoma cases. PTEN and p27 expressions decreased in hyperplasia and carcinoma cases with respect to proliferative endometrium. All these differences were statistically significant (P < 0.05). PTEN positively correlated to p27 (P < 0.05); however, neither was correlated with survivin. None of these genes were correlated with classical prognostic factors such as grade and myometrial invasion in endometrioid adenocarcinoma. However, mean survival was statistically significantly higher in PTEN-positive cases (46.6 vs 16.4 months) (P < 0.05). Survivin overexpression might be one of the important mechanisms in the development of endometrioid adenocarcinoma along with lost or decreased activity of PTEN and p27. However, survivin seems to exert its role in ways different from those of PTEN or p27 in the development of endometrioid adenocarcinoma. These findings on the role of survivin in endometrioid adenocarcinoma should be confirmed and the pathways through which survivin acts in endometrioid adenocarcinoma studied further with a larger sample size.
PMID: 16803539 [PubMed - indexed for MEDLINE]

- 王军臣
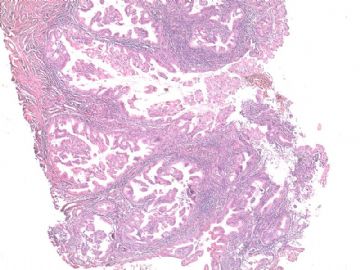
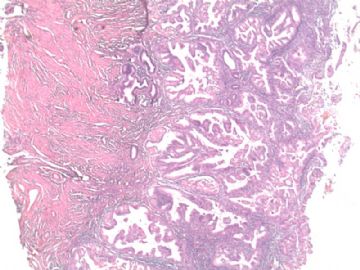
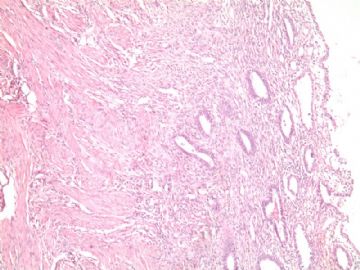
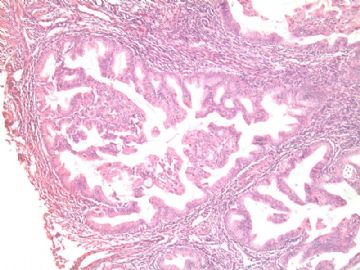
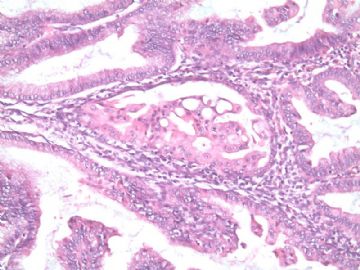
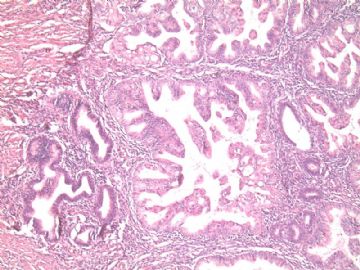
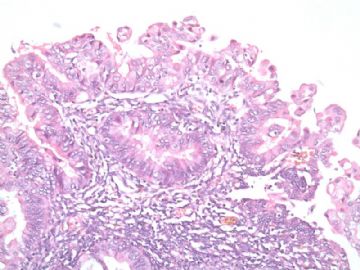
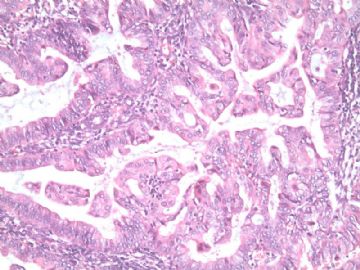
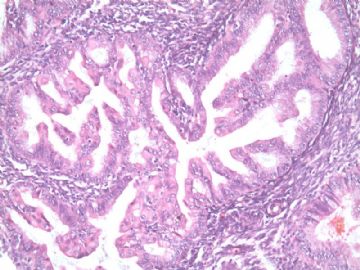
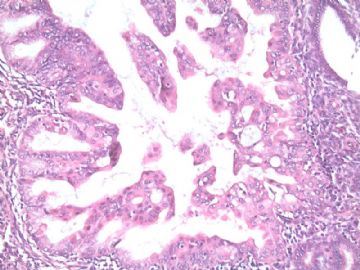
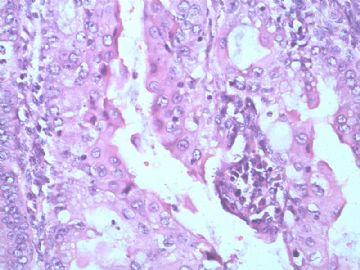
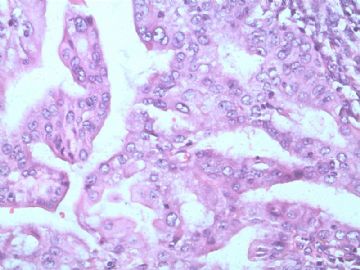




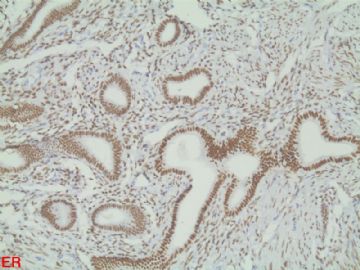
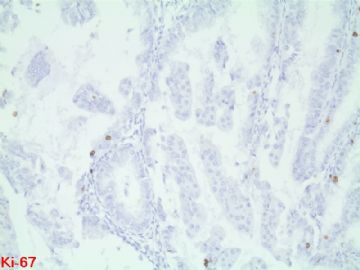





 。这种形态我最近连续遇到好几例,今天下午刚看过一例。
。这种形态我最近连续遇到好几例,今天下午刚看过一例。











