| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
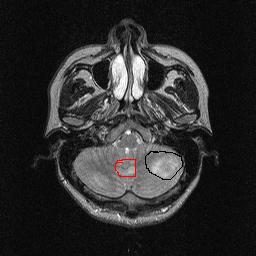
- 33岁男性,左小脑占位
-
本帖最后由 于 2006-10-31 15:50:00 编辑
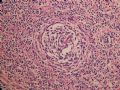
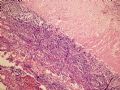
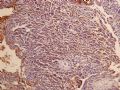
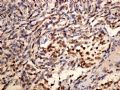
| 以下是引用mjma 在2006-10-31 12:57:00的发言: This is a difficult case to interpret. First of all, there seems to be two (not one) cerebellar lesions, and only the larger one was resected. In immunohistochemistry, the neoplastic cells have a very high MIB-1 labeling index, consistent with a malignant neoplasm. In addition, cells are immunoreactive to antibodies against NeuN, neurofilaments and MAP-2, all pointing towards neuronal differentiation. GFAP, EMA, and actin are negative. This argues against metastatic renal cell carcinoma, pilocytic astrocytoma, hemangioblastoma and clear cell meningioma. NeuN is a fairly new marker and recently, its specificity for neurons is questioned by reports describing its positive staining in non-neuronal cells. I am not very experienced in using NF-H or MAP-2. I now favor a metastatic malignancy of unclear classification (possible neuroendocrine differentiation), and suggest doing S100, HMB45, synaptophysin, chromogranin A, NSE and AE1 to further characterize this lesion. |
| 译: 这个病例很难解释。首先,有两个病灶而只切除了较大的一个病灶。免疫组化显示瘤细胞具有较高的核分裂指数,提示恶性肿瘤。另外,抗NeuN、NF和MAP-2的免疫反应提示神经元分化。GFAP、EMA和actin阴性,不支持肾细胞癌、毛细胞星型细胞瘤、血管母细胞瘤和透明细胞脑膜瘤。NeuN是个新近运用的抗体,其针对神经元的特异性最近遭遇质疑,有报道说在某些非神经元细胞也可出现阳性染色。NF-H和MAP-2两种抗体的运用我个人经验不是很丰富。我现在倾向于不明分类的转移性恶性肿瘤(可能具有神经内分泌分化),建议再做S-100、HMB45、Syn、CgA、NSE和AE1以进一步明确该病例特征。 |

- 靠树有断,靠墙有塌,靠命有失 所以我只能自强不息!!!!!!
-
This is a difficult case to interpret. First of all, there seems to be two (not one) cerebellar lesions, and only the larger one was resected. In immunohistochemistry, the neoplastic cells have a very high MIB-1 labeling index, consistent with a malignant neoplasm. In addition, cells are immunoreactive to antibodies against NeuN, neurofilaments and MAP-2, all pointing towards neuronal differentiation. GFAP, EMA, and actin are negative. This argues against metastatic renal cell carcinoma, pilocytic astrocytoma, hemangioblastoma and clear cell meningioma. NeuN is a fairly new marker and recently, its specificity for neurons is questioned by reports describing its positive staining in non-neuronal cells. I am not very experienced in using NF-H or MAP-2. I now favor a metastatic malignancy of unclear classification (possible neuroendocrine differentiation), and suggest doing S100, HMB45, synaptophysin, chromogranin A, NSE and AE1 to further characterize this lesion.

聞道有先後,術業有專攻
-
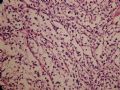
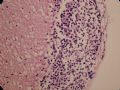
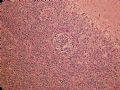
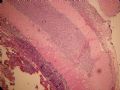
This is a difficult case to diagnose based on the information given so far. The photographed tumor appears to be located mainly on the leptomeningeal surface of the cerebellum, whereas the two MRI images show the discrete and well demarcated lesion to be intra-axial and not extra-axial (correct me if I am wrong). This makes me wonder whether the entire 3 x 3 cm resected tumorous tissue looks like the photos with only leptomeningeal tumor involvement and no bulkier and parenchyma-replacing neoplasm.
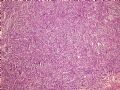
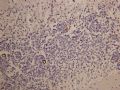
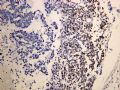
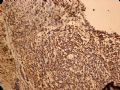
The neoplasm focally invades the cerebellar cortex by perivascular space permeation, but does not have a truly infiltrative growth pattern. The neoplastic cells show prominent clear cell fatures, and do not appear histiocytic. They raise the possibilities of (1) clear cell meningioma, (2) hemangioblastoma, (3) pilocytic astrocytoma, (4) oligodendroglioma, (5) PEComa (perivascular epithelioid cell tumor), and (6) metastasis.
Though the anatomic location is compatible, the neoplastic nuclei are larger than those encountered in clear cell meningiomas, and the characteristic broad collagenous fibers are lacking. Therefore I do not favor it being a case of clear cell meningioma. The lack of infiltrative growth is against the possibility of oligodendroglioma although rare oligodendrogliomas may be located mainly on the leptomeningeal surface and appear pedunculated grossly. The sinusoidal blood vessels in this case are different from the delicate capillaries in oligodendrogliomas.
As for the remaining differential diagnoses, I would need more information before planning for further diagnostic workup. Although no multivesiculated neoplastic stromal cells with large and indented hyperchromatic nuclei are seen, these characteristic cells may not be prominent in some hemangioblastoma. Metastastic malignancies are always difficult to rule out in the absence of clearcut glandular differentiation or keratinization or pertinent clinical history. Pilocytic astrocytomas of cerebellum often grow along the leptomeningeal surface and may show clear cells focally. Despite so, clear cells are never the only pattern seen in pilocytic astrocytomas. The perivascular invasion observed is quite interesting. This is nonspecific and can be seen in some gliomas (including pilocytic astrocytoma), meningiomas, and metastases. PEComas are rare mesenchymal tumors found in various locations that show myomelanocytic immunophenotype and may metastasize (including to the brain). They are associated with tuberous sclerosis, and primary PEComa in the brain has not been reported.
If all resected tissue look the same as this, diagnosis will rely much on immunohistochemistry. I would be delighted to learn more about this interesting case.

聞道有先後,術業有專攻