| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- NP (3) - Solitary tumefactive demyelinating lesion
-
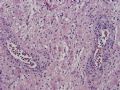
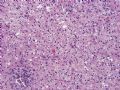
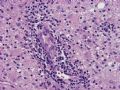
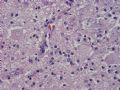
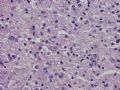
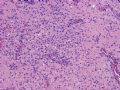
The following 16 photos are taken from a resected, ring-enhancing intra-axial mass in the left frontal lobe of a 51-year-old woman. What are your differential diagnoses? What additional stains would be helpful in your diagnostic workup?
-
本帖最后由 于 2006-11-01 10:06:00 编辑

聞道有先後,術業有專攻
This is a classic case of solitary tumefactive demyelinating lesion of brain. MRI images often show a ring-enhancing lesion surrounded by edema, a picture indistinguishable from glioblastoma, abscess, and other tumors (including metastasis). Many patients with this disease do not have a known history of multiple sclerosis (MS), but most will develop other lesions classic of MS.
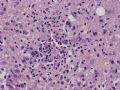
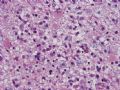
The lesion is well demarcated (Figures 1~4 in the first batch) and found in the white matter only. The cerebral cortex is spared (Figure 3). If deep gray matter (caudate nucleus, putamen, or thalamic complex) is involved, neurons are relatively spared and can be found scattered in the lesion. The lesion consists of a mixture of foamy macrophages, reactive astrocytes and blood vessels (Figures 5~8). Many macrophages have a tendency to accumulate around blood vessels (Figure 7). Some vessels may be cuffed by mononuclear inflammatory cells (mainly small lymphocytes) (Figures 9~10). Mitotic activity is observed in both phagocytic and glial (astrocytic) cells (Figures 11~12). For some reason, mitosis of some astrocytes may appear to be arrested at anaphase with condensed slender chromatids arranged in a radial fashion in the enlarged cell bodies - so-called Creutzfeldt cells (not specific for this disease, and can be seen in high grade astrocytomas, PML and other conditions) (Figure 11). The immediately adjacent white matter may contain many foamy macrophages (Figures 13~14). Sometimes, small aggregates of macrophages appear at lesional edge and mimic infarction (Figure 15). Rarely, microglial nodules are found (Figure 16).
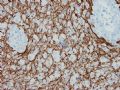
Using a combination of myelin stain (luxol fast blue/H&E) (Figures 1~3 in the second batch) and axonal stain (Bodian silver stain or neurofilaments immunostain) (Figures 4~6 in the second batch), marked loss of myelin with relative preservation of axons can be confirmed. I use the term "relative preservation" of axons because some axonal loss is inevitable with formation of axonal spheroids (Figure 5 in the second batch).
The main differential diagnoses of this lesion are (1) oligodendroglioma, (2) high grade (grade III and IV) astrocytoma, (3) infarct, (4) PML (progressive multifocal leukoencephalopathy), and (5) rare toxic/metabolic encephalopathies (such as chemotherapeutic agent [methotrexate and cyclophosphamide are prototypes]-induced toxic leukoencephalopathy, mitochondrial encephalopathy and various types of leukodystrophy). The most important of all these is of course oligodendroglioma. The abundance of foamy macrophages, associated blood vessels and scattered mitoses have led many pathologists down the wrong diagnostic path. The cytologic details of foamy macrophages and neoplastic oligodendrocytes are quite different under high power examination. The reactive astrocytes in this lesion may appear atypical and raise the possibility of astrocytoma. Though this is not an absolute rule, but finding abundant macrophages should always cast doubt on the diagnosis of glioma. Infarcted parenchyma shows coagulative necrosis that may contain scattered neutrophils and/or macrophages. Capillaries usually are lined by hypertrophied endothelia, and neurofilaments immunostain will not show any preserved axons in the lesion. PML lesions have myelin loss, associated macrophages, even the perivascular inflammation. As a rule, there will be large transformed astrocytes and characteristic, virally infected oligodendrocytes with enlarged nuclei containing ground-glass, amphophilic viral inclusion bodies within and adjacent to the lesion.

聞道有先後,術業有專攻
-
Figures 1~3 are taken from the interface (Figure 1) and center (Figures 2~3) of the lesion stained by the luxol fast blue/H&E method. Figures 4~6 are the same areas on a section stained immunohistochemically by an antibody against neurofilaments. What is your diagnosis?

聞道有先後,術業有專攻