1)Am J Surg Pathol. 2000;24:167-76.
Gastric dysplasia: the Padova
international classification.
Rugge M, Correa P, Dixon MF, Hattori
T, Leandro G, Lewin K, Riddell RH, Sipponen P, Watanabe H.
Department of Surgical and Oncological
Sciences, Università degli Studi di Padova, Italy.
Comment in: Am J Surg Pathol. 2001 May;25(5):694.
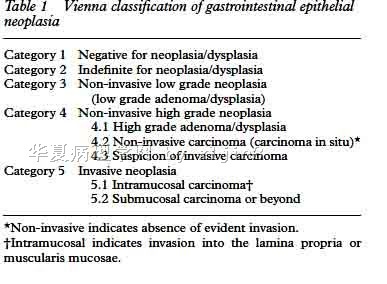
A worldwide-accepted histologic,
classification of the gastric carcinomatous and precancerous lesions is a prerequisite
for a consistent recording of epidemiologic data and for both
developing and evaluating primary and secondary preventive efforts. Different
nomenclatures have been proposed for gastric precancerous lesions in eastern
countries and in Japan. This article presents a classification of gastric precancerous
lesions resulting from an international consensus conference involving
pathologists of different countries. Five main diagnostic categories are identified.
To allow comparisons with the nomenclature proposed by the Japanese Research
Society for Gastric Cancer, each category was also assigned a numeric identification:
1 = normal, 2 = indefinite for dysplasia,3 = noninvasive neoplasia, 4 =
suspicious for invasive cancer, and 5 = cancer.The interobserver reproducibility of
the histologic classification was tested in a series of 46 cases. By collapsing benign
alterations (categories 1+2) versus noninvasive neoplasia (category 3)
versus suspicious for invasive cancer and fully appearing carcinomatous lesions
(categories 4+5), the general agreement value was 77.7%, whereas kappa
coefficient was 0.63. By examining gastric precancerous lesions from diverse
populations, the authors agreed that the gastric precancerous process is
universal and the differences in nomenclatures are merely semantics. The international
Padova classification of the gastric precancerous lesions is submitted to
the attention of the international scientific community, which is invited
to test and to improve on it.
2)Gut. 1999 Jul;45 Suppl 1:I5-8.
Gastric precancerous lesions: heading
for an international consensus.
Genta RM, Rugge M.
Departments of Pathology and Medicine,
Baylor College of Medicine and Veterans Affairs Medical Centre, Houston,
Texas, USA.
As pathological criteria lie at the
foundation for the classification of many diseases, a crucial requisite for such
classifications to be valid is that their morphological basis be standardised.
Inadequately standardised diagnostic criteria result in unacceptable
interobserver variation, a factor that may influence both individual patient care
and the evaluation of clinical protocols. One of the most important goals in
gastric diseases today is to establish whether cure of Helicobacter pylori is an
effective preventive measure against gastric cancer. To tackle this issue it is
necessary to measure reliably intermediate outcomes, specifically gastric atrophy
and dysplasia. However, there is little agreement on what gastric atrophy and
atrophic gastritis are, and treatment and follow up results obtained at one
clinical centre are often radically different from those obtained at another.
Similarly, studies that examine the fate of dysplastic lesions in the stomach show
a great divergence of outcomes between Europe and North America and Japan,
where the concept of dysplasia has different connotations. To reach a consensus on
the definitions and diagnostic criteria for atrophy and atrophic gastritis, a
group of gastrointestinal pathologists and gastroenterologists met in Houston,
Texas, USA, in February 1998. Substantive progress was made, but several
problems remained, and a study aimed at resolving the issues that seem to stand in the
way of an international agreement is currently underway. To fulfil the need
for a broad discussion on the diagnostic differences of gastric dysplasia and
cancer between East and West, an international group of pathologists
gathered in Padova, Italy, in the spring of 1998. Their main objectives were: (1)
to agree on the definitions of the spectrum of gastric preneoplastic lesions; (2)
to establish an international glossary for gastric precancerous lesions; and (3)
to test the consensus and eventually generate guidelines useful to clinicians
for the development of management strategies. A consensus was achieved
on the definition of gastric dysplasia as preinvasive neoplasia. Other
validation studies are underway. The experiences achieved in the search for an
international consensus on the phenotypes of atrophic gastritis and gastric
dysplasia may represent a model in dealing with the new scenario of a modern
evidence-based pathology.
3)Lancet. 1997;349:1725-9.
Differences in diagnostic criteria for gastric carcinoma
between Japanese and western pathologists.
Schlemper RJ, Itabashi M, Kato Y, Lewin KJ, Riddell RH,
Shimoda T, Sipponen P, Stolte M, Watanabe H, Takahashi H, Fujita R.
Department of Gastroenterology, Showa University Fujigaoka Hospital,
Yokohama-shi, Japan.
Erratum in: Lancet 1997
Aug 16;350(9076):524.
Comment in:Lancet. 1997
Aug 9;350(9075):448.
Lancet. 1997
Aug 9;350(9075):448.
Lancet. 1997
Jun 14;349(9067):1711-2.
BACKGROUND: There have been many studies on gastric
carcinoma in populations with contrasting cancer risks. We aimed to find out whether
the criteria for the histological diagnosis of early gastric carcinoma were
comparable in Western countries and Japan. METHODS: Eight pathologists from
Japan, North America, and Europe individually reviewed 35 microscope slides: 17
gastric biopsy samples and 18 endoscopic mucosal resections taken from 17 Japanese
patients with lesions ranging from early gastric cancer to adenoma, dysplasia,
and reactive atypia. The pathologists were given a list of pathological criteria
and a form on which they were asked to indicate the criteria on which they based
each diagnosis. FINDINGS: For seven slides most Western pathologists diagnosed
low-grade adenoma/dysplasia, whereas the Japanese diagnosed definite carcinoma in
four slides, suspected carcinoma in one, and adenoma in only two. Of 12 slides
with high-grade adenoma/dysplasia according to most Western pathologists
the Japanese gave the diagnosis of definite carcinoma in 11 and suspected in
one. Of six slides showing high-grade adenoma/dysplasia with suspected carcinoma
according to most Western pathologists the Japanese diagnosed definite carcinoma
in all. There were no major differences in the diagnoses of three slides
showing reactive epithelium
and seven slides with clearly invasive carcinoma. When
the opinion of the majority of the pathologists was taken as the final
diagnosis there was agreement between Western and japanese in 11 of the 35 slides
(kappa coefficient 0.15 [95% CI 0.01-0.29]). Presence of invasion was the most
important diagnostic criterion for most Western pathologists whereas for the Japanese
nuclear features and glandular structures were more important.
INTERPRETATION: In Japan, gastric carcinoma is diagnosed on nuclear and structural
criteria even when invasion is absent according to the Western viewpoint. This
diagnostic practice results in almost no discrepancy between the diagnosis of a
superficial biopsy sample and that of the final resection specimen. This may also
contribute to the relatively high incidence and good prognosis of gastric carcinoma
in Japan when compared with Western countries.
|