| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- Left neck mass
| 姓 名: | ××× | 性别: | Male | 年龄: | 41 |
| 标本名称: | Left neck mass, deep to the parotid gland | ||||
| 简要病史: | no significant history | ||||
| 肉眼检查: | outside consult, no gross photos | ||||
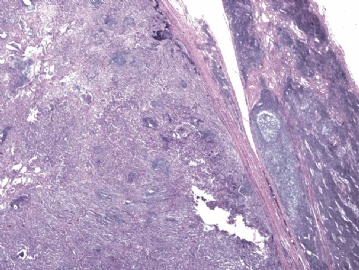
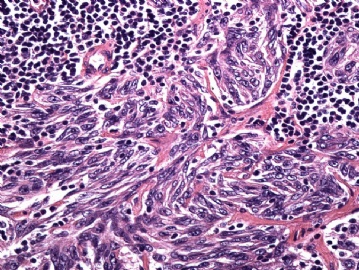
This is an outside consult case. The histology is very classic.
首先考虑:滤泡树突细胞肉瘤(follicular dendritic cell sarcoma,FDCS。
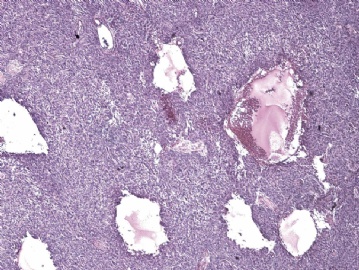
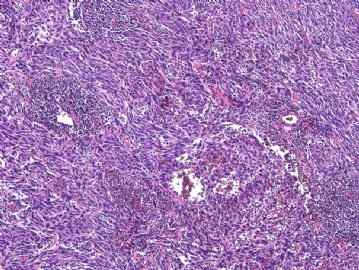
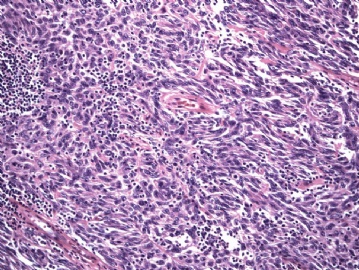
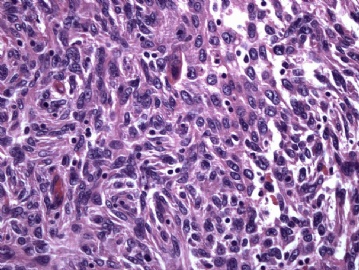
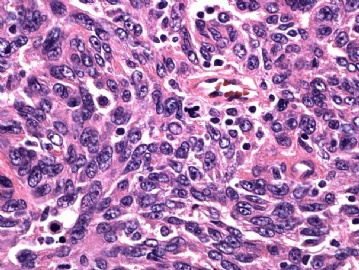
本例支持征有:(1)发生在颈部淋巴结。该处为最好发部。而且没啥症状;(2)梭形细胞为主,少数卵圆形细胞;(3)有胸腺瘤样和脑膜瘤样的结构,局灶可见旋涡状或编席状排列,低倍下可见小囊腔:(4)细胞核长梭形和短梭形多见,也见卵圆与卵圆核。泡状核或细颗粒状染色质,小核仁,少数大核仁,可见核分裂相;(5)一定程度的核异型。需要IHC标记CD21、CD23、CD35、Vim、fasin、D2-40阳性。也有少数其他的淋巴造血标志物表达。
正如Dr.Ma所述的交错突树突细胞肉瘤,FDCS与交错突树突细胞肉瘤(任何地方可以发生,临床可有发热、乏力、盗汗等症状,也可无症状;CD21、CD35、CD1a、S-100以及其他)形态表型有很大的重叠,很难鉴别,需要IHC标记来区分。
正如Dr.Jin所说,要与脑膜肿瘤、转移性肉瘤样癌(甚至恶黑)、梭形细胞变异性DLBCL鉴别,甚至与异位胸腺瘤相鉴别,需要适当配套抗体加以鉴别。

- 王军臣
| 以下是引用海上明月在2010-2-9 19:41:00的发言:
首先考虑:滤泡树突细胞肉瘤(follicular dendritic cell sarcoma,FDCS。 本例支持征有:(1)发生在颈部淋巴结。该处为最好发部。而且没啥症状;(2)梭形细胞为主,少数卵圆形细胞;(3)有胸腺瘤样和脑膜瘤样的结构,局灶可见旋涡状或编席状排列,低倍下可见小囊腔:(4)细胞核长梭形和短梭形多见,也见卵圆与卵圆核。泡状核或细颗粒状染色质,小核仁,少数大核仁,可见核分裂相;(5)一定程度的核异型。需要IHC标记CD21、CD23、CD35、Vim、fasin、D2-40阳性。也有少数其他的淋巴造血标志物表达。 正如Dr.Ma所述的交错突树突细胞肉瘤,FDCS与交错突树突细胞肉瘤(任何地方可以发生,临床可有发热、乏力、盗汗等症状,也可无症状;CD21、CD35、CD1a、S-100以及其他)形态表型有很大的重叠,很难鉴别,需要IHC标记来区分。 正如Dr.Jin所说,要与脑膜肿瘤、转移性肉瘤样癌(甚至恶黑)、梭形细胞变异性DLBCL鉴别,甚至与异位胸腺瘤相鉴别,需要适当配套抗体加以鉴别。 |
It seems that the 3 main considerations are 1) Follicular dendritic cell sarcoma (FDCS); 2) Interdigitating dendritic cell sarcoma (IDCS); 3) Thymoma.
The outside pathologist thinks that it is thymoma based on the cytokeratin positivity. I am also citing 2 classic papers of FDCS and IDCS. What do you favor based on morphology? I have immunostain results to follow.
1, Follicular dendritic cell sarcoma. Clinicopathologic analysis of 17 cases suggesting a malignant potential higher than currently recognized.
Chan JK, Fletcher CD, Nayler SJ, Cooper K.
Department of Pathology, Queen Elizabeth Hospital, Kowloon, Hong Kong.
BACKGROUND: The goal of this study was to characterize the clinicopathologic features of follicular dendritic cell sarcoma, a very uncommon neoplasm. METHODS: The 17 cases were collected from the consultation and surgical pathology files of the authors, including 8 previously reported cases. The histologic and immunohistochemical features and outcome were analyzed. RESULTS: The patients had a median age of 40 years, with a slight female predominance. Seven patients presented with enlarged lymph nodes, and ten presented with tumor in extranodal sites. Two cases were associated with hyaline-vascular Castleman's disease. The tumors had an average greatest dimension of 6.7 cm. The most common histologic feature was a storiform or fascicular array of spindle, ovoid, or polygonal cells with oval nuclei, delicate nuclear membrane, vesicular or granular chromatin, distinct nucleoli, indistinct cell borders, and frequently fibrillary cytoplasm. There were often scattered multinucleated forms. The tumor cells sometimes formed sheets, circular whorls, follicle-like structures, trabeculae, or pseudovascular spaces. There was a sprinkling of small lymphocytes, with or without cuffing around blood vessels. The neoplastic cells were immunoreactive for CD21 (17 of 17 cases), CD35 (17 of 17 cases), desmoplakin (10 of 17 cases), epithelial membrane antigen (14 of 16 cases), S-100 protein (6 of 17 cases), and CD68 (2 of 17 cases), but not cytokeratin. Ultrastructural studies showed villous processes connected by desmosomes. Only one harbored the Epstein-Barr virus. Among 13 patients with a median follow-up of 3 years, local recurrence occurred in 6, metastasis in 6, and 3 died of disease. CONCLUSIONS: Follicular dendritic cell sarcoma exhibits distinctive histologic features that permit its presumptive recognition, but a firm diagnosis requires confirmation with special studies. Because it has a significant recurrent and metastatic potential (the latter risk having been previously underestimated), it should be viewed as an intermediate grade malignancy. An intraabdominal location is associated with a particularly aggressive clinical course.
2. Interdigitating dendritic cell sarcoma. A report of four cases and review of the literature.
Gaertner EM, Tsokos M, Derringer GA, Neuhauser TS, Arciero C, Andriko JA.
Dept of Dermatopathology, 14th St and Alaska Ave NW, Bldg 54, Washington, DC 20307, USA.
To better define the clinical and pathologic features of interdigitating dendritic cell sarcoma (IDCS), we report 4 cases, including the first reported in the tonsil. There were 2 male and 2 female patients (mean age, 70 years). Sites of tumor included 1 case each in the right cervical lymph node, left axillary lymph node, right tonsil, and right inguinal lymph node. Histologically, all showed diffuse effacement of the lymphoid tissue by pleomorphic round to spindled cells with convoluted nuclei and abundant eosinophilic cytoplasm. All were immunoreactive for S-100, CD68, lysozyme, and vimentin. CD45 was positive in 3 cases and CD1a in 1 case. Fascin was positive in 3 cases. Other immunostains, including CD3, CD20, CD21, CD30, actin, cytokeratin, and HMB-45, were negative. Ultrastructurally, the tumor cells were elongated and showed indented nuclei, variable numbers of lysosomes, and interdigitating cytoplasmic processes. Follow-up was available for all cases. One patient died of widespread disease 2 months after diagnosis. One was alive with metastatic lung disease at 12 months. Two patients were disease free at 5 and 9 months.
-
Shangdongzhang, you brought the differential diagnosis of Angiomatoid Fibrous Hitiocytoma (AFH). That is very interesting. When I first looked at the case, AFH did cross my mind. I did not favor not diagnosis because the cells in AFH are usually more histiocytoid or myoid. The pseudoangiomatoid spaces are usually very prominent.
Here are the immunostains for the case.
S-100: Negative
CD68: Negative
Desmin: Negative
EMA: Negative
CD45: only stain those lymphocytes
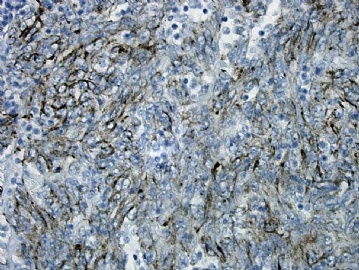
AE1/AE3: Focally positive, see picture 1
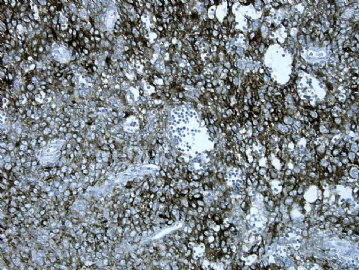
CD21: Positive picture 2
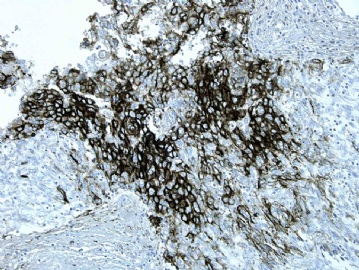
CD35: Positive picture 3
CD23: Positive picture 4
Clusterin: Positive picture 5
Thank you everybody for participating. Dr. Jin, you are very knowledgeble and up to date on literatures.
Our lab actually do not have CXCL13 antibody. Our D2-40 (mainly used for mesothelial cells and mesothelioma) stain has very high background, so I did not order it.