| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 挑战传统观念的卵巢肿瘤!
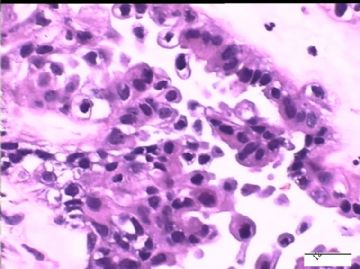
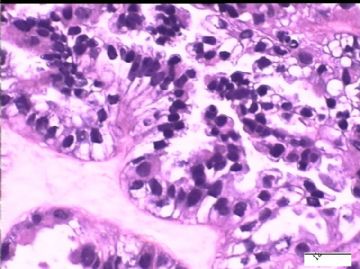
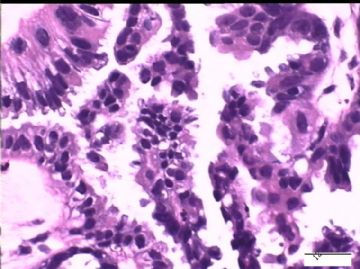
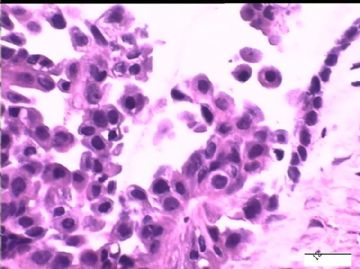
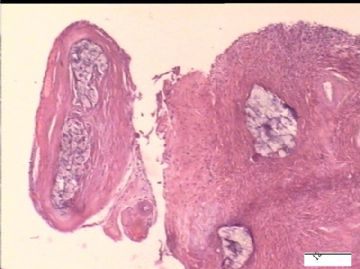
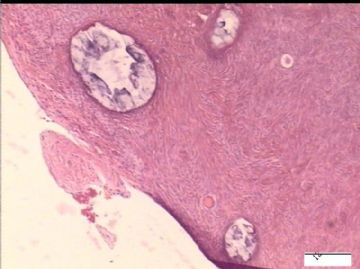
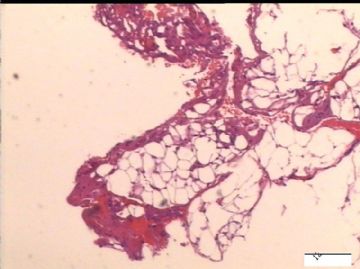
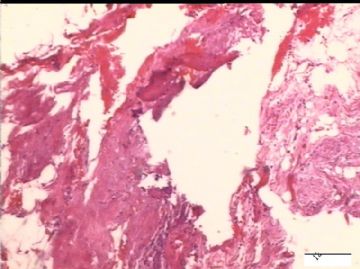
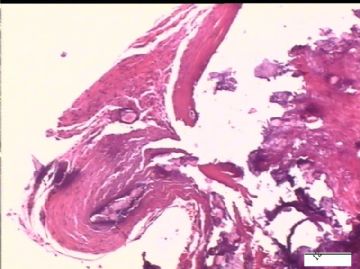
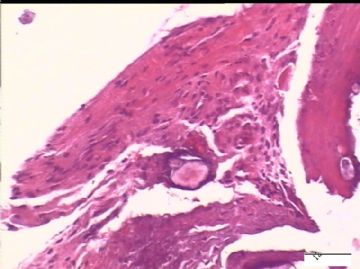
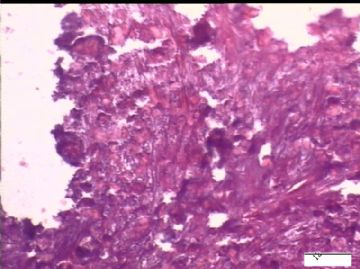
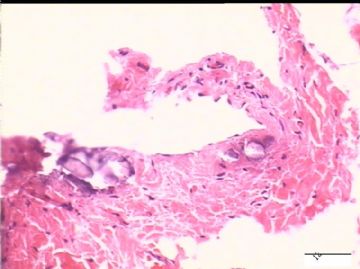
| 姓 名: | ××× | 性别: | 女性 | 年龄: | 31岁 |
| 标本名称: | 左侧卵巢间隔30天的2次活检 | ||||
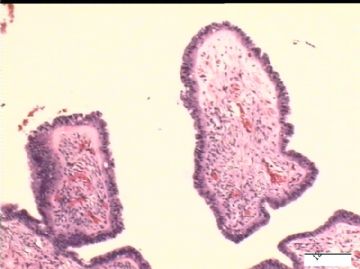
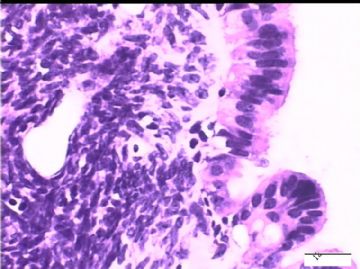
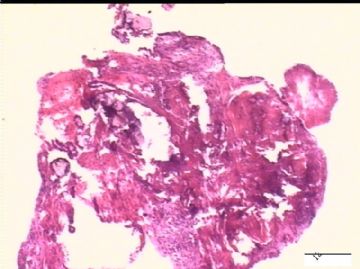
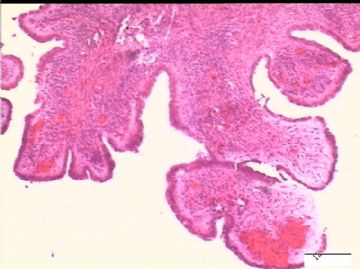
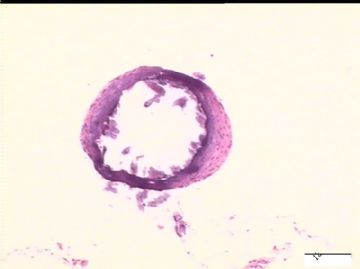
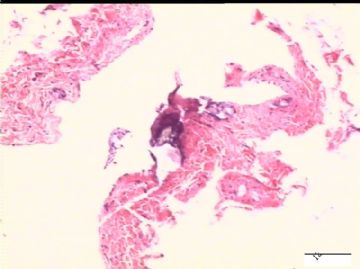
| 简要病史: | 试管婴儿,剖宫产手术中发现大网膜、盆腔腹膜、和双侧卵巢表面弥漫性颗粒状和乳头状病变(0.2-0.8 cm),类似非妇科肿瘤来源的转移癌。
请大家发表宝贵意见。谢谢! | ||||
| 肉眼检查: | |||||
-
本帖最后由 于 2010-01-13 09:02:00 编辑

- xljin8
-
本帖最后由 于 2010-01-21 04:03:00 编辑
| 以下是引用xljin8在2010-1-21 3:31:00的发言: 腹膜浆液性微乳头状瘤病(腹膜交界性浆液性肿瘤, Serous bordarline tumors of the peritoneum) 是非常罕见的女性原发性腹膜肿瘤,被推测起源于第二苗勒系统。文献报告最大组为17例临床病理分析。
Biscotti
CV, Hart WR. Peritoneal
serous micropapillomatosis of low malignant potential (serous borderline tumors
of the peritoneum). A clinicopathologic study of 17 cases.Am J Surg
Pathol. 1992;16:467-75. Department
of Pathology, Cleveland Clinic Foundation, OH 44195-5138. Primary
peritoneal serous micropapillomatosis of low malignant potential, or serous
borderline tumor of the peritoneum, is a relatively rare lesion that is histologically
indistinguishable from peritoneal "implants" associated with ovarian
papillary serous tumors of low malignant potential. We analyzed 17 cases to further define the pathologic
features and prognosis of this entity. The ages of the patients ranged from
16 to 67 years (mean, 33 years). Eight patients
were symptomatic with
chronic pelvic or abdominal pain (five patients), adnexal mass (one patient),
small-bowel obstruction (one patient), and possible endometriosis (one
patient). In nine cases
(53%), peritoneal serous micropapillomatosis of low malignant potential was an incidental finding
discovered during evaluation or treatment of other conditions. Grossly,
the peritoneal lesions were focal or diffuse. They commonly appeared as miliary granules and often were believed to
be peritoneal carcinomatosis. Microscopically,
peritoneal serous micropapillomatosis of low malignant potential had all of the
patterns seen in superficial("noninvasive") peritoneal implants of
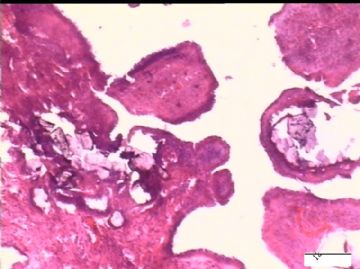
ovarian serous borderline tumors. Psammoma bodies
were a prominent feature of all cases. Twelve patients
also had typical endosalpingiosis. Most
patients were treated by hysterectomy and bilateralsalpingo- oophorectomy. Surgical treatment in seven patients consisted only of biopsy. Ten patients had residual
unresected disease at the time of their initial operation. Several
patients received adjuvant chemotherapy. Follow-up was available for 14 of the
17 patients. One patient
died of metastatic breast carcinoma at 3.8 years; another
patient died 7 weeks after operation, possibly as a complication of therapy.
The other 12 patients were alive at last known contact after follow-up
intervals of 8 months to 16.2 years (mean, 7.5 years). Two of these 12 patients
developed multiple episodes of small-bowel obstruction due to persistent
peritoneal serous micropapillomatosis of low malignant potential;neither
received adjuvant chemo- or radiotherapy. Both were
alive without progressive disease 10.9 and 16.2 years after initial diagnosis,
respectively. This excellent prognosis supports a
regimen of conservative therapy for these patients. 主要数据: 年龄:16-67岁,平均33岁 临床表现:有症状8例,其中5例为慢性盆腔/腹腔疼痛。因其他疾病偶尔发现9例。手术所见:局灶性或弥漫性腹膜表面粟粒状颗粒性病变,似癌症广泛转移(Carcinomatosis) 组织学观察:形态结构与非浸润性卵巢交界性浆液性肿瘤相同;砂砾体100%(17/17);输卵管内膜异位70.5%(12/17)。 治疗:全子宫+双侧附件切除8例;仅取活检9例;部分病例接受化疗或放疗。 随访:14/17例,时间8个月-16.2年,平均7.5 年。 结果:一例手术后7周死于并发症;一例3.8 年后死于乳腺癌转移;12例生存,最长者已生存16.2年。 结论:腹膜交界性浆液性肿瘤预后非常好,可保守治疗。 本例与其不同点:无砂砾体;手术后自行消退。 |

- xljin8
-
本帖最后由 于 2010-01-14 06:02:00 编辑
| 以下是引用天天田田在2010-1-14 5:41:00的发言: 我在一月前遇到一例剖宫产(23岁),卵巢囊实性肿块21*15*15cm,最后诊断:黏液性交界性肿瘤,伴局灶上皮内癌;当时曾怀疑与妊娠有关,建议患者去上海红房子会诊,结论与我们一致;患者也未作进一步治疗,目前还在随访中。 今天看到金老师的病例,也希望请教一下各位专家,在妊娠条件下,卵巢肿瘤的诊断是不是要适当退一退,不要过诊断?有无研究资料介绍妊娠与肿瘤的关系? 谢谢! 非常感谢您的参与,能否把您的病例发到网上一起讨论,谢谢! |

- xljin8
-
本帖最后由 于 2010-01-15 03:37:00 编辑
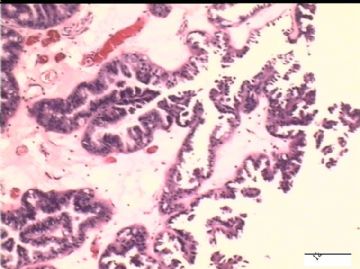
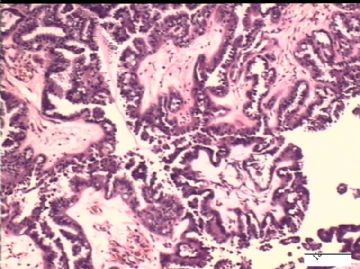
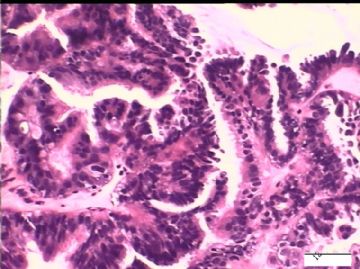
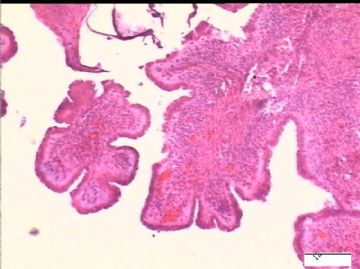
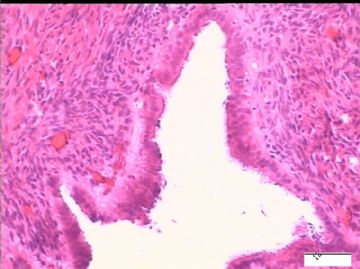
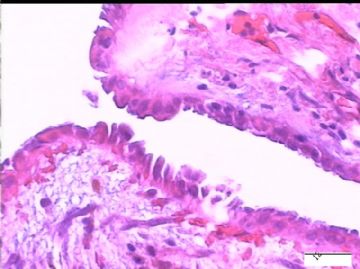
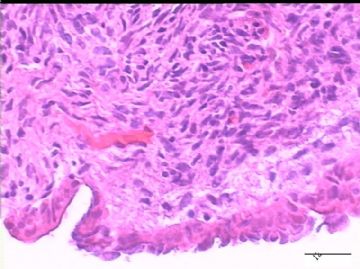
前后二次的共性为 卵巢(腹膜)表面乳头状腺纤维瘤。
复习PubMed有关卵巢腺纤维瘤文献,
其中最大一组为法国医生RNS, et al.在1993 年的研究报道。
Randrianjafisamindrakotroka
NS, Gasser B, Philippe E. CHU Majunga, Madagascar.[The malignant potential of
adenofibroma and cystadenofibroma of the ovary and mesovarium. 118
casesincluding 13 proliferative and 5 carcinomatous] J Gynecol Obstet Biol
Reprod. 1993;22:33-8.The relationship between adenofibroma and cystadenofibroma
and the frequency and features carcinomas developed on these benign tumours are
little known.Eight-hundred and forty-five epithelial tumours of the ovary
diagnosed over a 10-year period have been re-examined. One-hundred and eighteen
adenofibromas and cyst-adenofibromas were recorded. One-hundred were benign and
formed an architectural spectrum from which emerged: (1)surface papillary
adenofibroma accounting for 5% of the cases and appearing at a mean age of 27
years; (2) cystadenofibroma in 77.5% of the cases at a mean age of 53
years; (3)adenofibroma in 17.5% of the cases at a mean age of 64 years.
Adenofibroma was bilateral in 18 cases. Among the other cases were an
endometrioid cyst and two simple serous cysts. The cells were serous in 110
cases, mucinous in 6 cases and weakly acidophilic to clear in 2 cases. Eighteen
of these tumours were malignant:13 were associated with epithelial hyperplasia
and 5 with a carcinoma. The 13 adenofibromas with atypical epithelial
hyperplasia (at a mean age of 60 years) were all made of serous cells; 6 of
them were low-grade and 7 high-grade tumours with 3 microinvasions. One patient
died at the age of 78, of an unknown cause; the others are still alive after a
mean follow-up of 11.3 years. The 5 invasive carcinomas appeared on an
adenofibroma at the mean age of 70 years; 3 patients died (2 of metastases),
one is alive after 9 years and one was loss sight of.
主要数据为:
1)回顾性分析10年期间855例卵巢上皮性肿瘤,腺纤维瘤为118例(13.8%)
良性100例(84.7%),恶性18例(15.3%)。
2)表面乳头状腺纤维瘤5例(4.2%),平均年龄27 岁。囊性腺纤维瘤 77.5%, 平均年龄53岁;腺纤维瘤17.5%, 平均年龄64 岁。
3)单侧性100例;双侧性118例。
4)组织学分类:浆液性110例、粘液性6例、嗜酸-透明细胞型2例。
5)形态学良性100例;恶性118例。其中13例为上皮增生、5例有浸润(平均年龄70岁)。
6)随访结果:5例腺纤维瘤伴有浸润性癌的病例中3例死于肿瘤转移、1例手术后生存了9年;1例失访。
7)5例表面乳头状腺纤维瘤临床均为良性。
请教:表面乳头状腺纤维瘤的临床病理特点?此病例的治疗建议?
谢谢!

- xljin8
-
本帖最后由 于 2010-01-14 03:50:00 编辑
谢谢曹医生和Dr.wfbjwt的宝贵意见,要注意活检部位的差异、怀孕期长期高激素水平对微浸润的影响、和可能引起的A-S反应。
还有些临床情况向大家汇报。
1)剖宫产时,手术医生发现大网膜、盆腹膜、卵巢和邻近组织表面、膀胱表面都有弥漫性颗粒状病变,但是双侧卵巢的大小和形状并没有改变。
2)30天后,第二次手术中探查发现,绝大多数结节病灶都自发性消失了,仅双侧卵巢和盆腔粘连处(患者因慢性盆腔炎而不孕)有少量病变组织残留。本次活检部位比第一次广泛,包括左右二侧卵巢和盆腔腹膜。显微镜检查右侧卵巢病变仅表现为卵巢浅层有不钙化灶,无乳头状肿瘤样改变。左侧卵巢为表面乳头状肿瘤性病变。
请教的问题:
1)第一次手术所见的广泛性肿瘤性病变是交界性乳头状肿瘤的种植,还是腹膜原发性病变?
2)交界性乳头状病变的细胞异性、细胞内空泡、靴钉样改变是A-S反应吗?
3)经典型卵巢浆液性乳头状瘤合并妊娠是否可出现相同的组织学改变?
谢谢?

- xljin8