| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 31岁/女性,骨多发性病变,骨髓瘤?
-
本帖最后由 于 2010-01-04 15:09:00 编辑
这个年龄31岁多发股转移,乳腺癌一般是首选的,胃和肺等的也需要考虑。还有一个地方是卵巢等妇科来源的。
GCDFP本身也不是完全特异的(这个病例多少肿瘤细胞表达GCDFP? %),腮腺肿瘤,皮肤附属器官来源的, 还有肺癌(特别是腺癌,15%的腺癌可以表达,一般少于10%的肿瘤细胞阳性)等也是可以表达的。
不知道您们有不有mammaglobin? 虽然也不是对乳腺癌完全特异的, 但是如果阳性的话可以双保险。如果怀疑是多形性小叶癌, E-cadherin 应该是阴性的。 我想如果加上CK7,CK20, mammaglobin, E-cadherin, WT1 应该可以帮助进一步的确认是否是乳腺癌。
(我听说中国人的胃癌可以ER阳性, 不知道中国人的肺癌可不可以阳性?)
-
本帖最后由 于 2010-01-08 17:13:00 编辑
1. Eur J Cancer. 2009 Jul;45(11):1979-86. Epub 2009 Apr 15.
Lobular phenotype related to occult-metastatic spread in axillary sentinel node and/or bone marrow in breast carcinoma.
Vincent-Salomon A, Caly M, De Rycke Y, Fréneaux P, Klijanienko J, Laé M, Viard F,Nos C, Bidard FC, Alran S, Salmon R, Kirova Y, Pierga JY, Sigal-Zafrani B,Sastre-Garau X.
To determine whether any histological trait was associated with regional and/or systemic spread of occult tumour cells (OTCs) in small size invasive breast cancer, we compared tumour characteristics, axillary sentinel lymph node (SN) and bone marrow (BM) status in a series of 287 pT1T2 cases. Surgery was the first step of treatment, associated with SN procedure and with BM aspiration for the detection of OTC. SN was histologically classified as negative, metastatic (>2mm), micro-metastatic (>0.2mm and 2mm) or involved by OTC detected by immunohistochemistry (Ni+, 0.2mm). BM specimens were analysed after immunocytochemistry and classified as negative or positive with atypical cytokeratin-positive OTC. Metastasis and micro-metastasis in the SN were correlated with size, grade and vascular invasion. In contrast, presence of OTC in both SN and BM was independent of these parameters but positively associated with lobular type. This correlation was also observed for BM status, which was similarly independent of the tumour characteristics. No association was found between SN status and BM status. Our data indicate that, in the course of breast cancer, OTC spreading is frequent and could be an early event, related to lobular histological type but independent of classical histoprognostic parameters, and that the loco-regional metastatic spread of OTC is not a prerequisite for systemic involvement.
2. Ann Oncol. 2003 Jul;14(7):1072-7.
Occult central nervous system involvement in patients with metastatic breast cancer: prevalence, predictive factors and impact on overall survival. Miller KD, Weathers T, Haney LG, Timmerman R, Dickler M, Shen J, Sledge GW Jr.
BACKGROUND: As screening central nervous system (CNS) imaging is not routinely performed, the incidence and clinical relevance of occult CNS metastases in advanced breast cancer is unknown. PATIENTS AND METHODS: All patients screened for participation in one of four clinical trials were included; each of the trials excluded patients with known CNS involvement and required screening CNS imaging. A cohort of breast cancer patients with symptomatic CNS metastases was identified from the IU Cancer Center Tumor Registry for comparison. RESULTS: From November 1998 to August 2001, 155 screening imaging studies were performed. Twenty-three patients (14.8%) had occult CNS metastases. HER-2 overexpression (P = 0.02) and number of metastatic sites (P = 0.03) were predictive of CNS involvement by multivariate analysis. Median survival from time of metastasis (1.78 versus 2.76 years; P <0.0001) and from screening (4.67 versus 10.4 months; P = 0.0013) was shorter in patients with than without occult CNS metastasis. Survival among patients with occult CNS metastasis was similar to patients with symptomatic CNS disease. CONCLUSIONS: Patients with CNS involvement, whether occult or symptomatic, have an impaired survival. Occult CNS metastasis is relatively common, but impact on survival of treating occult CNS disease in patients with progressive systemic metastases is questionable.
3. Clin Breast Cancer. 2000 Oct;1(3):217-25.
Clinical relevance of occult metastatic cells in the bone marrow of patients with different stages of breast cancer.Janni W, Rjosk D, Braun S. Data are emerging about the prognostic relevance of occult metastatic cells in the bone marrow of patients with various solid tumors. Discrepancies among different studies on the prognostic relevance of isolated tumor cells may be caused by tumor cell heterogeneity and the use of different immunoassays. There is increasing evidence that validated anticytokeratin antibodies (e.g., A45-B/B3) represent the present standard for the detection of isolated tumor cells. This immunocytochemical assay allows the identification of patients with occult tumor cell dissemination that cannot be identified by conventional screening methods in tumor staging. According to recent studies, these patients are at higher risk for subsequent development of distant metastases and might therefore benefit from early systemic therapy. At advanced stages of the disease, the micrometastatic tumor load after adjuvant therapy, or at the time of emerging recurrences, appears to reflect the tumor's ability to progress. Therapeutic monitoring and cell-cycle independent antibody-based therapy are among possible implications of this new, promising diagnostic tool. The present review also focuses on state of the art, reliable detection methods of occult metastatic cells in the bone marrow of breast cancer patients and on the prognostic relevance of these cells at different stages of the disease.
4. Ann Oncol. 2002 Mar;13(3):422-9. Human mammaglobin RT-PCR assay for detection of occult breast cancer cells in hematopoietic products. Silva AL, Tomé MJ, Correia AE, Passos-Coelho JL.BACKGROUND: The aim of this study was: (i) to evaluate the sensitivity and specificity of mammaglobin as a reverse transcriptase polymerase chain reaction(RT-PCR) marker of breast cancer cells; (ii) to determine the incidence of tumor cell contamination of hematopoietic samples from patients with breast cancer.
MATERIALS AND METHODS: A nested RT-PCR assay for mammaglobin was developed.Sensitivity was determined by serial dilution assays with breast cancer cell lines, human breast cancers and normal breast tissue. Specificity was evaluated in hematopoietic samples from healthy volunteers and patients with hematological malignancies or solid tumors other than breast cancer. RESULTS: The mammaglobin transcript was detected in all 15 breast cancers, one benign breast tumor and five normal breast tissues studied, as well as in three breast cancer cell lines,in dilutions as low as 10(-8). The transcript was not detected in any of 47 peripheral blood samples, 15 bone marrow aspirates and 28 peripheral blood progenitor cell samples from the three control populations. Mammaglobin mRNA was detected in 19 of 78 peripheral blood samples from patients with breast cancer starting systemic chemotherapy, as well as in five of 30 repeat samples collected before the fourth cycle of treatment. The transcript was also present in six of seven bone marrow aspirates from patients with metastatic disease, two of five with loco-regional disease, but not in the aspirate of two patients with thrombocytopenia and a previous history of breast cancer. CONCLUSIONS: Human mammaglobin mRNA is a sensitive and specific marker of breast cancer cells and should be further studied as a molecular marker of tumor cell contamination of hematopoietic tissues.
5. Cancer Res. 2001 Dec 15;61(24):8845-50.
Detection of occult metastatic breast cancer cells in blood by a multimolecular marker assay: correlation with clinical stage of disease.Taback B, Chan AD, Kuo CT, Bostick PJ, Wang HJ, Giuliano AE, Hoon DS.Department of Molecular Oncology, John Wayne Cancer Institute, Santa Monica, California 90404, USA.
Currently, molecular markers offer the unique opportunity to identify occult metastasis in early stage cancer patients not otherwise detected with conventional staging techniques. To date, well-characterized molecular tumor markers to detect occult breast cancer cells in blood are limited. Because breast tumors are heterogeneous in tumor marker expression, we developed a "multimarker" reverse transcription-PCR assay combined with the highly sensitive electrochemiluminescence automated detection system. Breast cancer cell lines (n = 7), primary breast tumors (n = 25), and blood from normal donors (n = 40) and breast cancer patients [n = 65; American Joint Committee on Cancer (AJCC) stages I-IV] were assessed for four mRNA tumor markers: beta-human chorionic gonadotropin (beta-hCG), oncogene receptor (c-Met), beta1-->4-N acetylgalactosaminyl-transferase, and a tumor-associated antigen(MAGE-A3). None of the tumor markers were expressed in any normal donor bloods.Breast cancer cell lines and primary breast tumors expressed beta-hCG, c-Met,beta 1-->4-N-acetylgalactosaminyl-transferase, and MAGE-A3 mRNA. Of the 65 breastcancer patient blood samples assessed, 2, 3, 15, 49, and 31% expressed 4, 3, 2,1, and 0 of the mRNA tumor markers, respectively. At least two markers were expressed in 20% of the blood specimens. The addition of a combination of markers enhanced detection of systemic metastasis by 32%. In patient blood samples, the MAGE-A3 marker correlated significantly with tumor size (P = 0.0004) and AJCC stage (P = 0.007). The combination of beta-hCG and MAGE-A3 mRNA markers correlated significantly with tumor size (P = 0.04), and the marker combination c-Met and MAGE-A3 showed a significant correlation with tumor size (P = 0.005) as well as AJCC stage (P = 0.018). A multimarker reverse transcription-PCR assay that correlates with known clinicopathological prognostic parameters may have potential clinical utility by monitoring tumor progression with a blood test.
6. Breast Cancer Res. 2001;3(5):285-8. Epub 2001 Jun 28.
Recent advances in technologies for the detection of occult metastatic cells in bone marrow of breast cancer patients. Braun S, Harbeck N.
Approximately half of breast cancer patients with stage I-III disease will suffer metastatic disease despite resection with tumour-free margins. In 30-40% of these patients, individual carcinoma cells can already be detected at the time of primary therapy in cytological bone marrow preparations using immunocytochemistry. Numerous prospective clinical studies have shown that the presence of occult metastatic cells in bone marrow is prognostically relevant to patient survival. Only a few studies failed to do so, thus stimulating a critical discussion on the methodology and clinical value of bone marrow analysis. The potential for obtaining improved prognostic information on patient outcome, for monitoring tumour cell eradication during adjuvant and palliative systemic therapy, and for specifically targeting tumour biological therapies are intriguing clinical opportunities that may be afforded by bone marrow analysis. Standardized and robust methodology is a prerequisite for clinical application of these techniques, however.
7. Biomed Pharmacother. 2001 May;55(4):229-42.Occult metastasis. Hawes D, Neville AM, Cote RJ.
The most important factor affecting the outcome of patients with invasive cancers is whether the tumor has spread, either regionally (to regional lymph nodes) or systemically. However, a proportion of patients with no evidence of systemic dissemination will develop recurrent disease after primary 'curative' therapy. Clearly, these patients had occult systemic spread of disease that was undetectable by methods routinely employed (careful pathological, clinical, biochemical and radiological evaluation). In addition, the success of adjuvant therapy is assumed to stem from its ability to eradicate occult metastases before they become clinically evident [1]. Therefore, methods for the detection of occult metastases in patients with the earliest stage of cancer, i.e., prior to detection of metastases by any other clinical or pathological analysis, have received a great deal of attention.
8. N Engl J Med. 2000 Feb 24;342(8):525-33.
Cytokeratin-positive cells in the bone marrow and survival of patients with stage I, II, or III breast cancer.
Braun S, Pantel K, Müller P, Janni W, Hepp F, Kentenich CR, Gastroph S, Wischnik A, Dimpfl T, Kindermann G, Riethmüller G, Schlimok G.
N Engl J Med. 2000 Feb 24;342(8):580-1.N Engl J Med. 2002 Aug 15;347(7):538-9; author reply 538-9.
BACKGROUND: Cytokeratins are specific markers of epithelial cancer cells in bone marrow. We assessed the influence of cytokeratin-positive micrometastases in the bone marrow on the prognosis of women with breast cancer. METHODS: We obtained bone marrow aspirates from both upper iliac crests of 552 patients with stage I, II, or III breast cancer who underwent complete resection of the tumor and 191 patients with nonmalignant disease. The specimens were stained with the monoclonal antibody A45-B/B3, which binds to an antigen on cytokeratins. The median follow-up was 38 months (range, 10 to 70). The primary end point was survival. RESULTS: Cytokeratin-positive cells were detected in the bone marrow specimens of 2 of the 191 control patients with nonmalignant conditions (1percent) and 199 of the 552 patients with breast cancer (36 percent). The presence of occult metastatic cells in bone marrow was unrelated to the presence or absence of lymph-node metastasis (P=0.13). After four years of follow-up, the presence of micrometastases in bone marrow was associated with the occurrence of clinically overt distant metastasis and death from cancer-related causes (P<0.001), but not with locoregional relapse (P=0.77). Of 199 patients with occult metastatic cells, 49 died of cancer, whereas of 353 patients without such cells, 22 died of cancer-related causes (P<0.001). Among the 301 women without lymph-node metastases, 14 of the 100 with bone marrow micrometastases died of cancer-related causes, as did 2 of the 201 without bone marrow micrometastases (P<0.001). The presence of occult metastatic cells in bone marrow, as compared with their absence, was an independent prognostic indicator of the risk of death from cancer (relative risk, 4.17; 95 percent confidence interval, 2.51 to 6.94; P<0.001), after adjustment for the use of systemic adjuvant chemotherapy. CONCLUSIONS: The presence of occult cytokeratin-positive metastatic cells in bone marrow increases the risk of relapse in patients with stage I, II, or III breast cancer.
9. Surg Oncol Clin N Am. 1997 Oct;6(4):683-98.
Systemic treatment for stage I and stage II breast cancer.
Hudis CA, Borgen P.
Department of Medicine, Memorial Sloan-Kettering Cancer Center, New York, New
Breast cancer presents as two interrelated problems. The first is disease in the breast and axillary lymph nodes and the second is metastatic spread to distant sites. Local diseases can be controlled with less morbidity than in the past
because of advances in surgery and radiotherapy. In addition, heightened public awareness and the more widespread use of mammography have increased the detection of smaller cancers that have a better prognosis and are easier to treat. The problem of late relapse leading to death, however, motivates continued intensive
study of systemic therapy as treatment for the undetectable micrometastatic disease remaining after surgery. Currently, hormonal therapy and chemotherapy are known to prolong disease-free and overall survival in nearly all groups of patients, although the relative and absolute influences of drug therapies are modest and vary among patient subgroups, and the proper application of these treatments to the hundreds of thousands of patients diagnosed worldwide per year could have a major impact on public health. For the future, clinical trials and
laboratory advances indicate that novel dosing and scheduling of chemotherapy agents combined with newer modalities may provide even greater impact against occult disseminated disease.
10. Cancer. 1996 Jul 1;78(1):10-6.
Polymerase chain reaction in the detection of micrometastases and circulating tumor cells.
Ghossein RA, Rosai J.
Department of Pathology, Memorial Sloan-Kettering Cancer Center, New York, New York 10021, USA.
Comment in:
BACKGROUND: The sensitive detection of circulating tumor cells and micrometastases may have important therapeutic and prognostic implications. METHODS: The molecular detection of occult tumor cells can be accomplished by amplifying tumor specific abnormalities present in the DNA or mRNA of malignant cells with the polymerase chain reaction (PCR). This approach has been used mainly for hemato-lymphoid malignancies. The other main PCR strategy for the detection of minimal residual disease (MRD) involves amplification of
tissue-specific mRNA. This method was applied for the detection of occult disease in solid tumors. RESULTS: PCR was shown to be superior to conventional techniques in detecting circulating tumor cells and micrometastases allowing the identification of 1 tumor cell diluted with 10(6)-10(7) normal cells. The central question of whether PCR positivity reliably predicts relapse remains unanswered for many tumor types. Serial analysis of a large number of samples is needed and currently undertaken in many institutions. CONCLUSIONS: PCR is a highly sensitive method for the detection of circulating tumor cells and micrometastases in solid and hematopoietic malignancies. If PCR positivity is found to be a reliable tool, this will likely have a major impact on the treatment of many cancers. Patients could be selected for systemic therapy at an earlier stage when the metastatic
tumor burden is low. PCR may improve the preoperative staging of patients with epithelial malignancies and therefore help avoid unnecessary radical procedures. Furthermore, this test may be useful in monitoring the effectiveness of adjuvant therapy, the intensity and duration of which is tailored to the individual patient. The impact of this PCR based approach on clinical oncology is likely to be profound.
11. Cancer. 1992 Dec 15;70(12):2831-4. CA 15-3 in patients with locoregional and metastatic breast carcinoma.
Geraghty JG, Coveney EC, Sherry F, O'Higgins NJ, Duffy MJ.
Department of Surgery, St. Vincent's Hospital, Elm Park, Dublin, Ireland.
BACKGROUND. The value of circulating CA 15-3 levels was assessed in 129 patients with recurrent breast carcinoma. METHODS. Patients were divided into four subgroups, according to the following: Group A, locoregional recurrence alone; Group B, locoregional and subsequent systemic recurrence; Group C, combined
locoregional and systemic recurrence; and Group D, differing sites of systemic disease. RESULTS. One of 14 patients with locoregional disease alone had increased levels of CA 15-3 (> 25 U/ml). However, 96% of patients (22 of 23 patients) with combined local and systemic disease had increased tumor marker levels. The difference in CA 15-3 levels in patients with combined disease compared with patients with local disease alone was statistically significant (117.0 versus 17.5 U/ml, respectively; P < 0.02). Twenty-four patients with locoregional recurrence later had distant metastasis develop. In this group, patients with an increased CA 15-3 value had a significantly shorter lead time to the development of distant metastases compared with patients with normal tumor marker levels (20.8 +/- 3.3 versus 10.3 +/- 2.7 months, respectively; P < 0.03). CA 15-3 values at diagnosis were increased in 88% of 115 patients with metastatic disease. There was no significant difference in CA 15-3 levels among metastases
to lung, liver, and bone nor was there any difference between single and multiple sites of distant metastasis. CA 15-3 is an excellent marker for systemic recurrence of breast carcinoma. CONCLUSIONS. Increased levels and no clinical evidence of recurrence strongly indicate the presence of occult metastatic disease.
12. Anticancer Drugs. 1992 Oct;3(5):455-62.
Bone metastasis in breast cancer.
Theriault RL, Hortobagyi GN.
Department of Medical Oncology, (Breast Medical Oncology), University of Texas,
MD Anderson Cancer Center, Houston 77030.
Bone metastases in breast cancer are common and frequently lead to serious skeletal related morbid complications. Metastases develop in areas of metabolically active trabecular bone. It is presumed that breast cancer cells
undergo the same stepwise process for metastases development as demonstrated in other tumor types. The specific factor or factors responsible for the osteotropism of breast cancer have not been identified. The morbid events
associated with skeletal metastases, such as pathologic fracture, and spinal cord compression, may be assessed objectively by a variety of techniques including skeletal radiography, radionuclide scanning, computed tomographic scanning and magnetic resonance imaging. Biochemical parameters or markers of skeletal
metastases are not sensitive enough to detect clinically occult disease. Therapeutic interventions for bone metastases include local and systemic therapies. Surgery and radiation therapy are most frequently used for relief of
pain or impending fracture, or when bone fracture or neurologic compromise has already developed. Systemic treatment of bone metastases appears to be as effective as systemic treatment of other metastatic sites. Both hormone and chemotherapy may provide significant palliation. Clinical research suggests that the adjunctive use of bisphosphonates may significantly reduce the incidence of skeletal-related morbid events associated with osteolytic bone disease. Future research efforts directed at determining the osteotrophic factors responsible for bone metastases in breast cancer, the pathophysiology of the bone remodeling process in metastatic disease and the prophylactic use of bisphosphonates may lead to significant clinical benefit for those in whom bone metastases from breast cancer develop.
13. J Clin Gastroenterol. 1988 Apr;10(2):213-7.
Occult carcinoma of the breast masquerading as primary adenocarcinoma of the small intestine. A case report.
Hansen RM, Lewis JD, Janjan NA, Komorowski RA.
Department of Medicine, Medical College of Wisconsin, Milwaukee. A fifty-year-old woman with abdominal pain, diarrhea, and weight loss ultimately required exploratory laparotomy. The entire small intestine was extensively
infiltrated by poorly differentiated adenocarcinoma; mesenteric lymph nodes and surrounding omentum were involved, but no extragastrointestinal tumor was found. A presumptive diagnosis of unresectable primary carcinoma of the small bowel was made. Chemotherapy was initiated with 5-fluorouracil 300 mg/m2/day by continuous intravenous infusion. Nine months later a left breast mass with multiple ipsilateral axillary and supraclavicular lymph nodes developed; biopsy revealed a poorly differentiated adenocarcinoma morphologically identical to the tumor involving her small bowel. In spite of breast irradiation and systemic hormonal therapy, the patient deteriorated rapidly and died from progressive metastatic disease.
14. J Neurosurg. 1985 Feb;62(2):227-33.
Intramedullary spinal cord metastasis. A clinicopathological study of 13 cases.
Costigan DA, Winkelman MD.
A retrospective autopsy study of 627 patients with systemic cancer disclosed 153 patients with metastasis to the central nervous system (CNS) and 13 patients with intramedullary spinal cord metastasis (ISM). Thus, the frequency of ISM was 8.5% of cases of metastasis to the CNS and 2.1% of all cases of cancer. Bronchogenic
carcinoma accounted for 11 cases of ISM, and breast carcinoma and melanoma for the other two. There were two distinct patterns of spinal cord involvement, indicating spread of tumor to the cord by two different routes. In nine of the 13 ISM patients a metastasis was found deep within the spinal cord, unassociated with leptomeningeal carcinomatosis; this most likely resulted from hematogenous spread of tumor from a pulmonary source. In the other four patients there was focal or multifocal direct extension of leptomeningeal metastatic tumor across
the pia into the parenchyma of the cord. Only four of the 13 patients had a clinical myelopathy; in three of these four this was the presenting feature of an occult lung cancer.

- xljin8
-
本帖最后由 于 2010-01-03 21:23:00 编辑
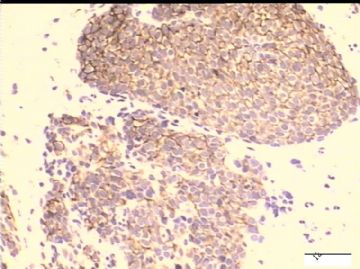
对了!转移性乳腺低分化癌。
我的标记抗体包括乳腺、肝脏、肾上腺、神经内分泌、肾脏、肺、淋巴造血、浆细胞、间皮、肌源性、恶黑、神经;几乎覆盖了我能想到的抗体。
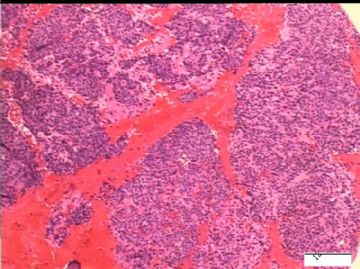
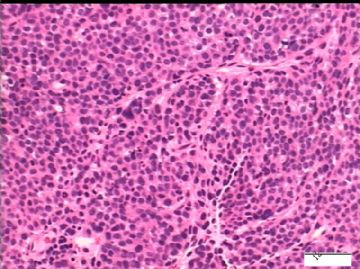
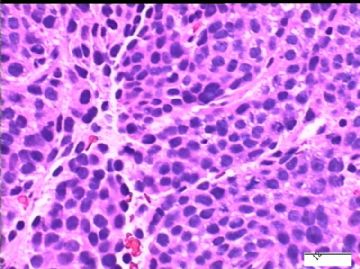
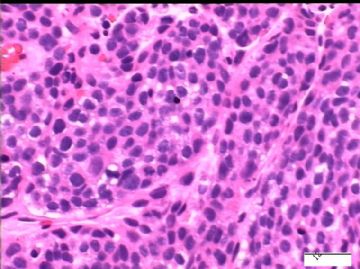
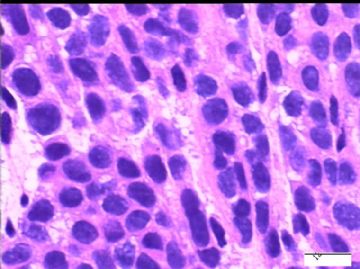
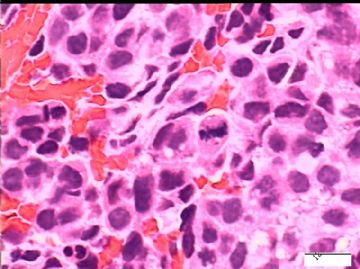
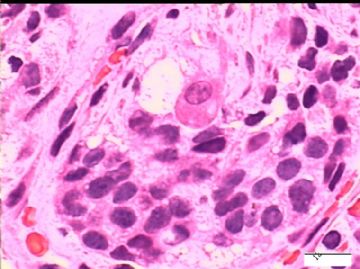
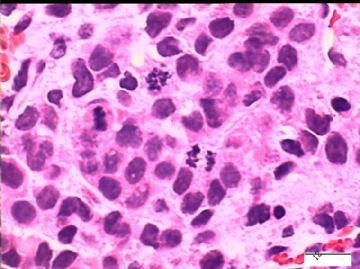
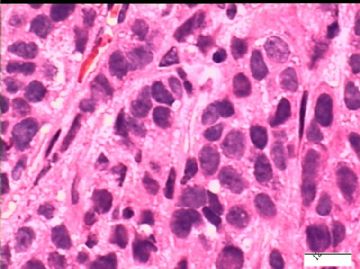
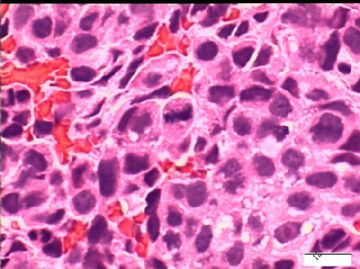
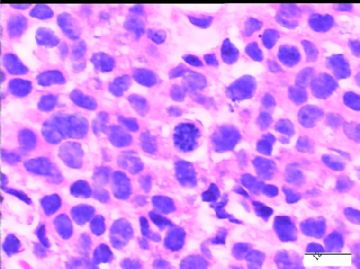
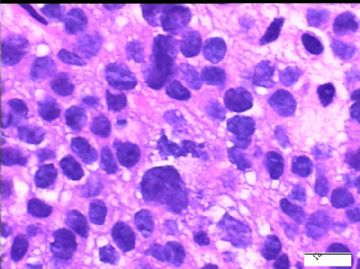
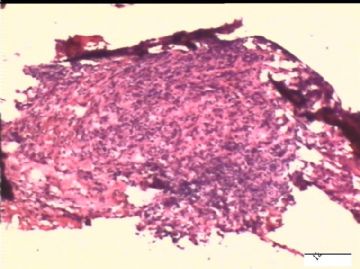
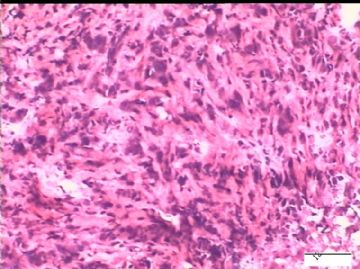
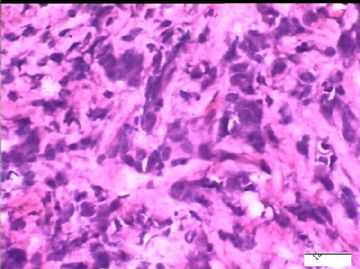
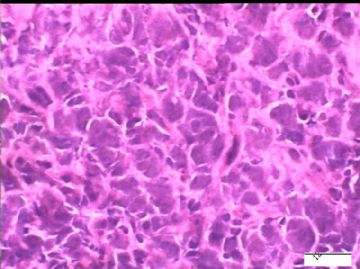
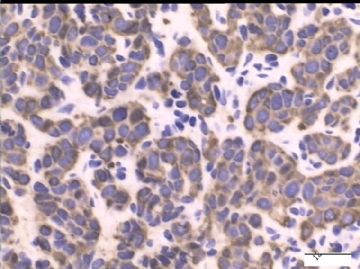
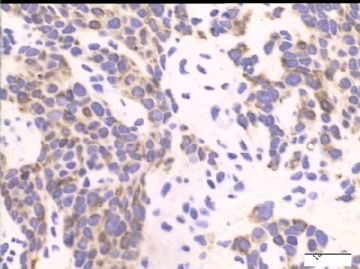
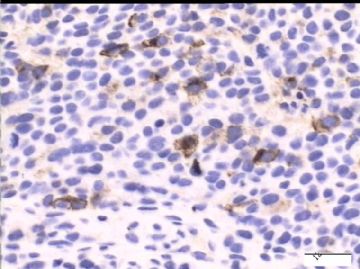
此例形态特点:
1)实体性细胞巢和小梁;
2)细胞形态比较一致性;
3)核分裂象多;
4)无腺管、鳞状上皮、神经内分泌分化特点;
5)无坏死;
临床上无明显的肿块,仅仅是PET/CT示骨的多发病病变、左侧腋下淋巴结高代谢、双侧胸腔积液。
根据此例的临床和病理特点,首先考虑转移性癌。来源呢?肾上腺、肝脏、乳腺(多形性小叶癌)、肺.....。
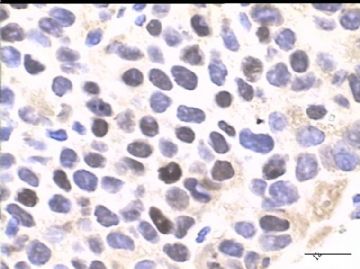
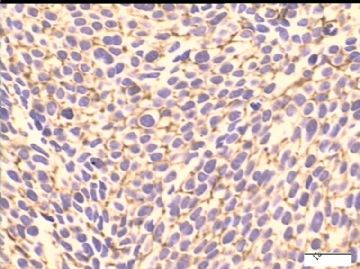
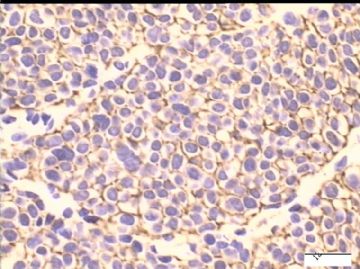
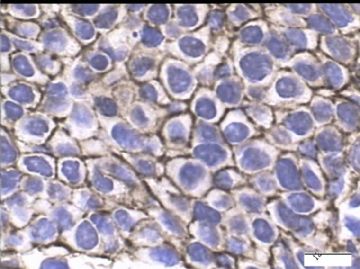
此例IHC表达:AE1/AE3(图1)、EMA(图2)、34BE12(图3)、GCDFP-15(图4-5)、ER(图6)。
要注意:CD138 很多癌可阳性表达!
再问病史,患者5个月前曾B超检查乳腺,无异常发现。住院时体检无肿块。
但血浆CA153异常升高。
我推测为乳腺隐性癌(Occult Carcinoma), 进一步检查和IHC标记是明天的工作了。
谢谢大家的帮助!

- xljin8