| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
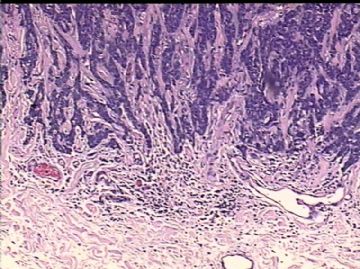
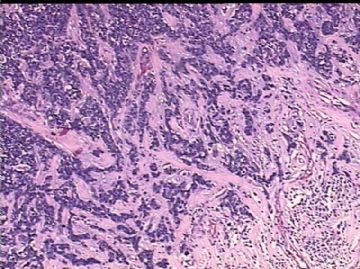
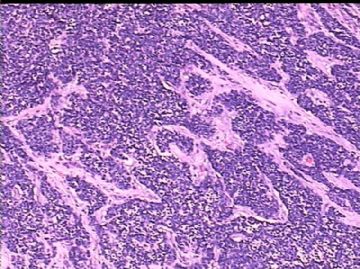
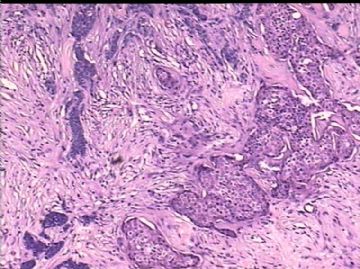
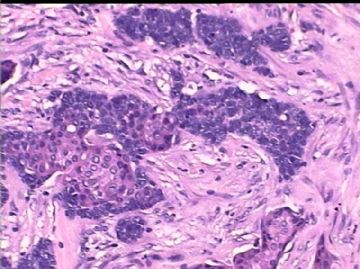
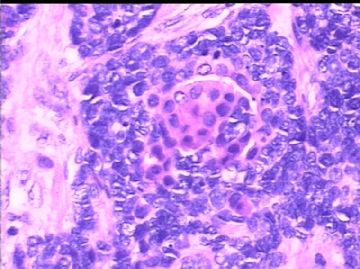
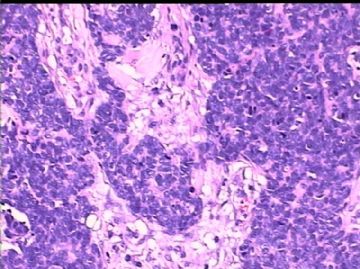
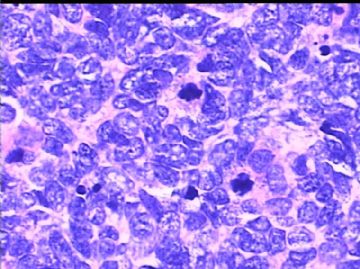
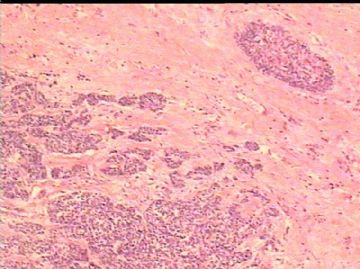
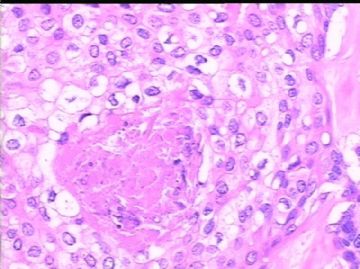
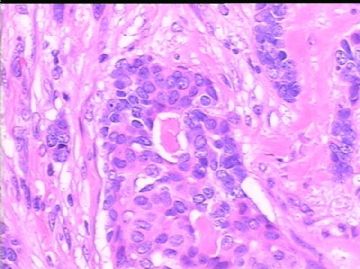
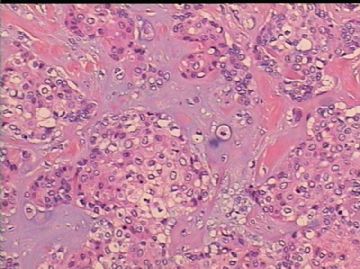
- B2300乳腺癌,类型?
| 以下是引用XLJin8在2009-12-18 18:07:00的发言:
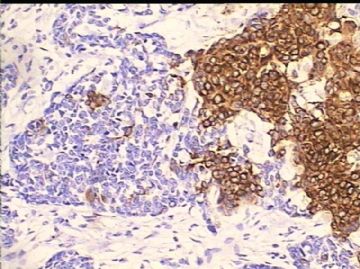
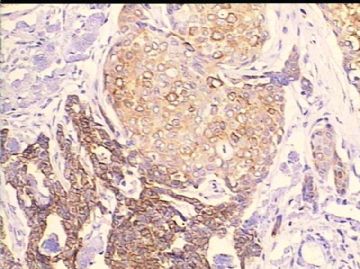
Dr. Chao,您好! 非常感谢您的意见。 有关乳腺原发性小细胞癌的病例报道非常少,最大组为Shin和Rosen的9例,“Small cell carcinoma of the breast. A clinicopathologic and immunohistochemical study of nine patients. Am J Surg Pathol 2000;24:1231-1238。很抱歉,一开始没把NSE+ Crg-A+的图给出。我们还将做电镜,看看小细胞是否有神经内分泌颗粒。此外再标记一些其它的神经内分泌标记物。
|
I am almost convinced by you. Many breast tumors can be focally positive for neuroendocrine markers.
Waiting for your EM result.
Thank you for sharing the interesting case.
-
本帖最后由 于 2009-12-19 12:44:00 编辑
Dr. Zhao,您好!
非常感谢您的意见。 有关乳腺原发性小细胞癌的病例报道非常少,最大组为Shin和Rosen的9例,“Small cell carcinoma of the breast. A clinicopathologic and immunohistochemical study of nine patients. Am J Surg Pathol 2000;24:1231-1238。很抱歉,一开始没把NSE+ Crg-A+的图给出。我们还将做电镜,看看小细胞是否有神经内分泌颗粒。此外再标记一些其它的神经内分泌标记物。
|
抗体 |
9例标记结果 |
|
AE1/AE3 Cam5.2 CK7 CK19 CK20 Vimentin NSE Crg-A Syn Calcitonin Leu7 Gastrin releasing peptide Neurofilament Somatostatin Seretonin ER PR Her2/neu Bcl-2 CD56 P53 |
9/9 8/9 7/9 7/9 0/9 4/9 9/9 4/9 5/9 3/9 3/9 2/9 0/9 0/9 0/9 6/9 5/9 0/9 9/9 7/9 6/9 |

- xljin8
Dr. XLJin8,
Your knew brest ca categories in details. Primary small cell carcinoma (SCC) is rare. I once saw one at AFIP. It was a classic case like lung or cervical scc. So I do not have much experience about scc. There is no large study in this area. It is true that the cytomorphologic features of this tumor share some similarity with classic scc. However, geneally we hope to see some good positivity for neuroendocrine markers before we call scc, such as ck56, chromogranin, synaptophysin,, NSE. This case is negative for CD56, CD57, synaptophysin. I did not see other neuroendocine marker positive also. Your case shows squamous differentiation. It may be scc, but I am not convinced now. If you want to have a unique diagnosis you must feel very comfortable for your dx. You have to exclude other reasonable diagnoses. Clinicians, patient and other patholoigsts will challenge your dxianosis.
I still favor the interpretaion of invasive ductal ca with basal-like phenotype and focal squamous differentiation. It can explain all morphologic and IHC features.
Sometime the simple or familar diagnostic term is easier to be accepted for most people especially in the situation without much difference for treatment.
Just for your reference,
Glad to know you in the web and thank for sharing your challenge case.
cz
-
本帖最后由 于 2009-12-16 05:11:00 编辑
| 以下是引用zhaoyan2006在2009-12-15 22:42:00的发言: 是否可以用化生性癌解释,不了解乳腺小细胞癌,请多讲解,我等长见识。
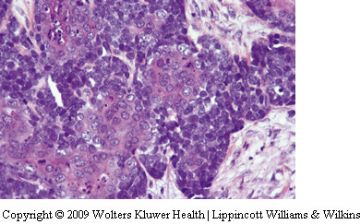
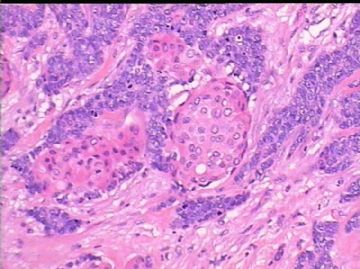
您的提问非常好,为什么不称为化生性癌? 试作解答: 乳腺化生性癌定义:一组异质性的由腺癌与梭形细胞、鳞状细胞、软骨样和骨分化成分区域相互混杂为基本特征的乳腺恶性肿瘤。病理学化生的基本概念为由一种分化成熟的细胞转变为另一种分化成熟的细胞。传统上用于腺上皮细胞,如胃粘膜的肠上皮化生(腺上皮-腺上皮)、支气管和宫颈柱状细胞的鳞状上皮化生(腺上皮-鳞状上皮)、肌上皮细胞的粘液软骨样化生(上皮-间叶)。在乳腺腺上皮细胞和/或肌上皮细胞也可发生表型的改变(化生),其本质是控制细胞表型分化的密码分子去抑制(de-repression)。鳞状化生可出现在乳腺的良性病变,如乳头状瘤、纤维腺瘤、囊肿、男性乳腺发育;也可出现在乳腺癌(3.7%),如浸润性导管癌或小叶癌。 请注意约16%的乳腺髓样癌可出现鳞状化生,但是并不称为化生性癌,而认为是髓样癌中的一种变异型,尽管髓样癌形态很凶险,免疫表型通常为3阴(ER-PR-cerbB2-),但预后却意外的好。 AFIP乳腺化生性癌的组织学分类 1纯上皮型癌 1.1鳞状上皮癌 1.1.1大细胞型,角化型或非角化型 1.1.2鳞状上皮癌伴梭形细胞化生(伴或不伴有棘皮细胞改变) 1.2腺鳞癌 1.2.1高分化 1.2.2低分化 1.2.3腺鳞癌伴梭形细胞化生 2混合性上皮和间叶癌 2.1癌伴有软骨分化 2.2癌伴有骨分化 2.3癌伴有横纹肌肉瘤成分 2.4癌肉瘤 您的观察非常仔细,其实图片中有一张是软骨化生的照片。在我目前复习的所有文献中并没有一篇讲到乳腺原发性小细胞癌伴有软骨成分。 最后回答为什么不称为化生性癌的原因:1)乳腺原发性小细胞癌是与髓样癌绝然相反的高度恶性的肿瘤;2)小细胞癌的起源可能为乳腺神经内分泌细胞或多功能干细胞,而不是腺上皮细胞或肌上皮细胞。就本例耒说,主要成分为未分化小细胞,又有鳞状细胞、小腺管结构、透明细胞、CD10+细胞(肌上皮?)、导管内癌、和软骨分化,更加倾向于肿瘤起源于多能干细胞。 由于乳腺原发性小细胞癌是乳腺癌中最罕见的类型,您可理解为肺外的小细胞癌。 谢谢您的提问! |

- xljin8
-
zhaoyan2006 离线
- 帖子:139
- 粉蓝豆:42
- 经验:301
- 注册时间:2009-02-23
- 加关注 | 发消息
-
本帖最后由 于 2009-12-14 06:08:00 编辑
| 以下是引用cqzhao在2009-12-11 4:07:00的发言: Bottomline: it is triple negative invasive ca. Question is the terminology. There is no much difference in term of clinical management. Stromal-like component is positive for CK7. All components are ca. By definition: Triple negative and some basal marker positive (ck5/6). It is basal-like ca. I do not know the meaning of negative E-cad. I would like to call invasive ductal ca with basal-like phenotype and focal squamous differention. Clearly squamous component is present. Some one may consider metaplastic ca. Basal-like ca and metaplastic ca are two different classification systems. In fact most cases of metaplastic ca are basal-like ca by definition. Just for your reference. Thank for sharing your case with us. cz 感谢Dr. Zhao 的诊断建议。我想诊断“乳腺原发性小细胞癌”如何?因为乳腺原发性小细胞癌(BSCC)是最罕见的乳腺癌。自1983年 Wade 等首例乳腺原发性小细胞癌报道以来,至今英文文献中的记载不到40例。 其中日本报道最多,英国2004年才有首例报道,我国还未见报道。非常想听您的高见。谢谢! |

- xljin8
Bottomline: it is triple negative invasive ca. Question is the terminology. There is no much difference in term of clinical management.
Stromal-like component is positive for CK7. All components are ca.
By definition: Triple negative and some basal marker positive (ck5/6). It is basal-like ca. I do not know the meaning of negative E-cad.
I would like to call invasive ductal ca with basal-like phenotype and focal squamous differention.
Clearly squamous component is present. Some one may consider metaplastic ca. Basal-like ca and metaplastic ca are two different classification systems. In fact most cases of metaplastic ca are basal-like ca by definition.
Just for your reference.
Thank for sharing your case with us. cz
-
本帖最后由 于 2009-12-11 03:54:00 编辑
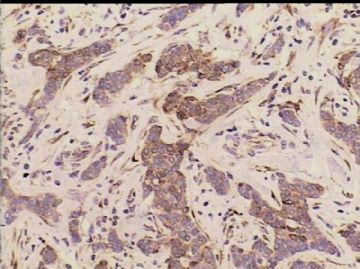
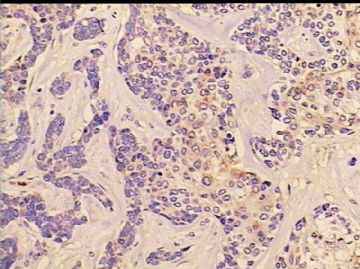
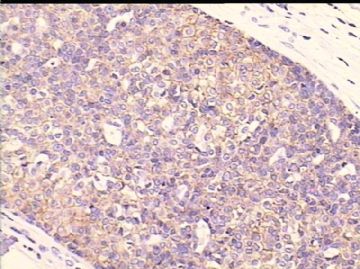
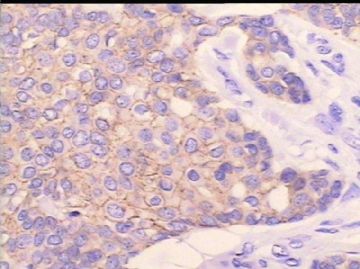
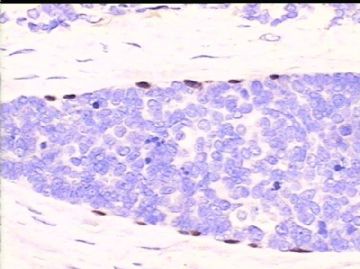
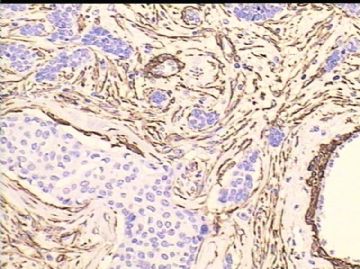
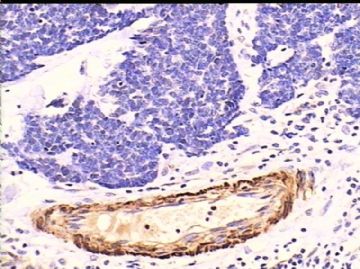
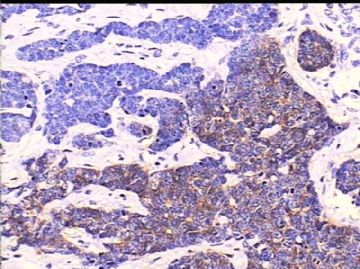
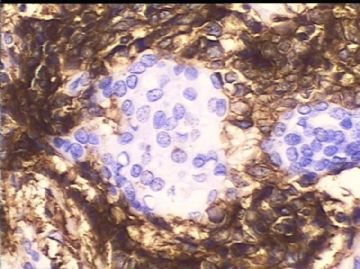
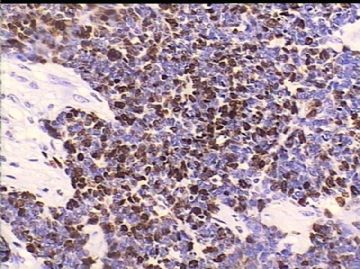
| 以下是引用cqzhao在2009-12-9 1:49:00的发言: Zhi Ding for more oppinion. Waiting for 楼 主 's IHC. Thanks Dr. Zhao, 您好! 将部分IHC照片附上, 请提宝贵意见, 谢谢! 增加其他区域 HE 照片1-4; 5)CK5/6;6)CK7;7)P63; 8)SMA;9)Calponin;10)CD10 11)CD10;12)Ki-67。 其他标记:AE1/AE3+,Cam5.2+,E-cadherin-/+,ER-PR-cerbB2-,CD56-CD57-SYN-, BRCA-2-/+,34BE12-,S-100-。 |

- xljin8