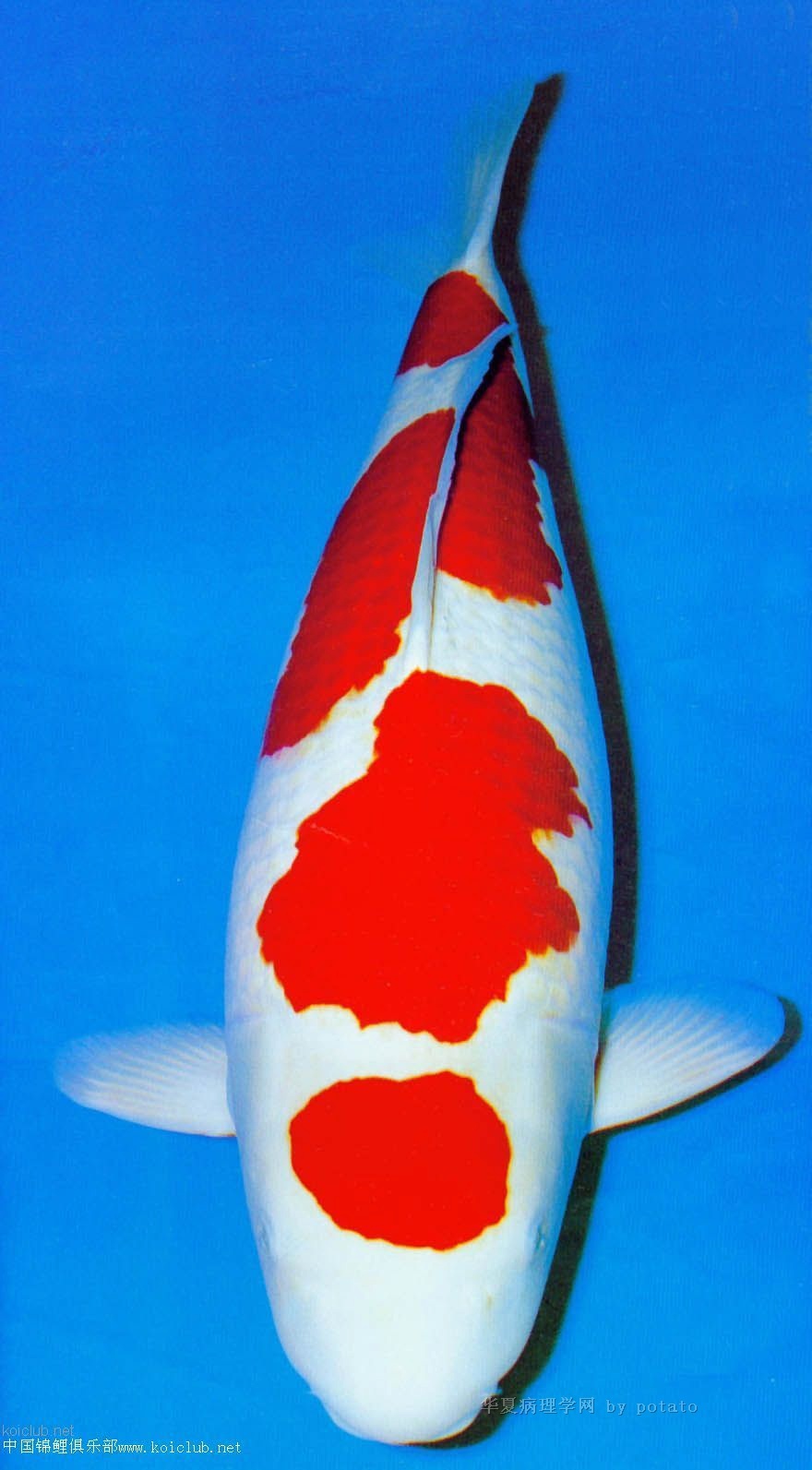
| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 50岁腹水,是间皮还是癌?请老师会诊(已确诊:低分化腺癌)
赵老师的第一个贴子:回顾一些病例,许多都有同样的问题,是间皮还是腺癌。这也确实是我们日常工作中在体液样本中最常见也最关键的问题,如果我们能做一些染色那么对大多数病例来说这也是一个简单的问题。
对于这类的体液样本我们似乎会想到所有不同的可能,并且去鉴别。
对胸膜或腹膜积液:
1。如果我不能100%确定是良性,我会做calretinin (间皮)和 BerEp4 (或其它上皮标记)染色。
2。如果calretinin是阳性BerEp4是阴性,那么细胞是间皮,然后我们去想是反应性的还是恶性的。
3。如果calretinin是阴性BerEp4是阳性,那么通常是转移腺癌。
4。如果是不明原发灶的转移性腺癌,我将在病人年龄、病史、影像、性别等基础上做一些染色去尽量寻找原发灶。如果患者是女性我会做CK7/CK20, ER (gyn, breast), TTF-1 (lung) 染色,当然不同的个体判读结果可能不同。
5。如果考虑淋巴肿瘤,我会首先做LCA ,CD3, CD20 ,然后再判断。。。
我们不能说可能是间皮或腺癌,我们要找到支持你诊断的依据。
给大家参考!
当然我也知道对基层单位来说做免疫组化是困难的,那就另当别论了。你只需要尽你最大的努力去证明你的阐述。一些病例可以请有经验的细胞学专家会诊。在这样的条件下你最好是不做出明确的诊断。
|
以下是引用cqzhao在2009-9-17 19:48:00的发言: 有时回顾本专栏部分话题,发现很多病例都是相同的争论——间皮还是腺癌?的确,这是我们日常工作中关于体液样本诊断碰到的最常见也是最主要的问题。其实,如果我们做一些标记,这种鉴别对大多数病例只是个简单的问题。看来我们对体液样本诊断的思维方式和处理方法完全不同。在胸膜或腹膜液: 1、如果我没有100%把握这是个良性病变,我会做calretinin (间皮)和 BerEp4 (或其它上皮性标记) 染色; 2、如果calretinin 阳性而BerEp4阴性,那这是间皮细胞,然后要考虑的是:反应性还是恶性? 3、如果calretinin 阴性而BerEp4阳性,那通常是转移癌; 4、如果这是个不知道原发灶的转移癌,就需要根据患者年龄、病史、影象、男/女等做部分染色来尽可能找寻原发灶。如果是个女性病人,常做的染色包括CK7/CK20, ER (妇科,乳腺), TTF-1 (肺)等。当然不同情况会选择不同的抗体组合。 5、如果考虑淋巴瘤,我首先选择LCA 、CD3及CD20 ,然后再决定。。。 我们不能说这可能是腺癌或间皮,我们需要证据来支持我们的诊断。 仅供参考。 当然,我知道某些基层医院做免疫染色可能很难,这就另当别论了,你必需尽最大努力甚至有时凭运气来做判断。部分病例即使对有经验的细胞病理学家也是富于挑战,这种情况下,你的最佳选择是不要做明确诊断。 很好的思路和处理问题方式,谢谢赵老师。 Occasionally reviewed some topics in this section. There are many cases with the same question, 间皮or adenocarcinoma. It is true this is the most common and key question in our daily practice for body fluid specimens. It is a very easy question for most of the cases if we can do some stains. Seems that we have totally different ways to think and handle theses kinds of body fluid specimens. In pleural or peritoneal fluid: 1. If I am not 100% sure it is a benign case, I will do calretinin (间皮)and BerEp4 (or other epithelial markers) stain. .2.If calretinin is positive and BerEp4 is negative, the cells are 间皮. Then we need to think it is reactive or malignant. 3. If calretinin is negative and BerEP4 is positive, generally it is a metastatic carcinoma 4. If it is a metastatic carcinoma with unknown primary, I will do some more stains based on the patient's age, history, imaging, male/female and try to figure out the primary. If patient is a women the stains often include CK7/CK20, ER (gyn, breast), TTF-1 (lung) et al. Of cause the panel can be different based on individual situation. 5. If lymphoid malignant is considered, I will stain LCA and CD3, CD20 first. Then decide .... We cannot say it may be adenocarcinoma or 间皮. We need evidence to support our diagnosis. For your reference.Of cause I know immuno stains may be difficult for some local hospitals. Then it is another story. You have to try your best and luck to make your interpretation. Some cases can be challenge for experienced cytopathologists. In this situation, it is better you do not make your definite diagnosis.
|
-
wangdingding 离线
- 帖子:1474
- 粉蓝豆:98
- 经验:6042
- 注册时间:2006-10-19
- 加关注 | 发消息
Occasionally reviewed some topics in this section. There are many cases with the same question, 间皮or adenocarcinoma. It is true this is the most common and key question in our daily practice for body fluid specimens. It is a very easy question for most of the cases if we can do some stains.
Seems that we have totally different ways to think and handle theses kinds of body fluid specimens.
In pleural or peritoneal fluid:
1. If I am not 100% sure it is a benign case, I will do calretinin (间皮)and BerEp4 (or other epithelial markers) stain.
.2.If calretinin is positive and BerEp4 is negative, the cells are 间皮. Then we need to think it is reactive or malignant.
3. If calretinin is negative and BerEP4 is positive, generally it is a metastatic carcinoma
4. If it is a metastatic carcinoma with unknown primary, I will do some more stains based on the patient's age, history, imaging, male/female and try to figure out the primary. If patient is a women the stains often include CK7/CK20, ER (gyn, breast), TTF-1 (lung) et al. Of cause the panel can be different based on individual situation.
5. If lymphoid malignant is considered, I will stain LCA and CD3, CD20 first. Then decide ....
We cannot say it may be adenocarcinoma or 间皮. We need evidence to support our diagnosis.
For your reference.
Of cause I know immuno stains may be difficult for some local hospitals. Then it is another story. You have to try your best and luck to make your interpretation. Some cases can be challenge for experienced cytopathologists. In this situation, it is better you do not make your definite diagnosis.