本帖最后网站上的诊断是这样的;是原网作者观点;不代表本人和华夏网任何个人观点。请自由引用。(以下内容我不提供翻译;请大家自由引用和翻译——大家一起学专业和英文)
Cytologic diagnosis: Epithelial Cell Abnormalities: Carcinoma, consistent with known clinical history of Paget's disease.
Biopsy diagnosis: Bx of vulva, same day as cytology: Poorly Differentiated Adenocarcinoma with Pagetoid spread. Bx of lower vulva 5 days later: Extramammary Paget's disease and Invasive Adenocarcinoma. Vulvar excision one month later: Infiltrating Poorly Differentiated Adenocarcinoma with overlying Paget's disease
Case provided by: Long Island Jewish Medical Center Lab, New Hyde Park, NY
Etiology:
Paget's disease can be located at various sites including the nipple, eyelid, axilla, perianal region, mons pubis, glans penis, and the vulva. Paget's disease of the vulva is associated with a higher than normal incidence of other malignancies, breast cancer being the most common. Histologically all of the sites are similar; however they seem to have a different morphogenesis. Mammary Paget's disease is almost always associated with intraductal or invasive ductal carcinoma of the breast. It is thought that there is a migration of malignant cells thru both the mammary and lactiferous ducts which result in invasion of the epidermis. Compared to the vulvar type in which 70% of cases have only purely intraepidermal carcinoma with only the remaining 30% having an in situ or invasive adnexal carcinoma.
Clinical Features:
Paget's disease of the vulva has been reported in women ranging from 38-87 years of age with an average age of 67. This disease predominately affects white postmenopausal women. Chief complaints, commonly present for many years, include pruritis, irritation, a burning sensation, and localized discomfort. The most commonly affected site is the labia majora. The lesions are erythematous, eczematous and indurated. They are often ulcerated and bleed easily on contact.
Cytology:
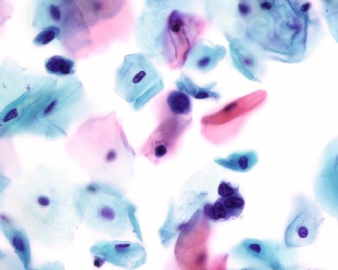
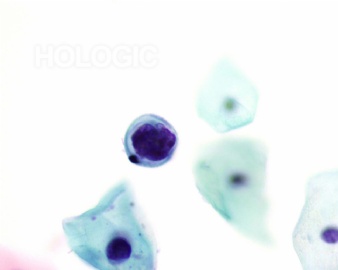
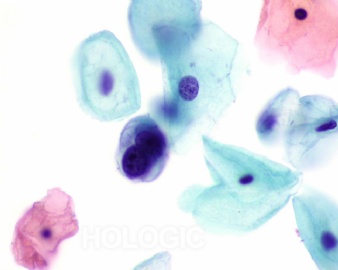
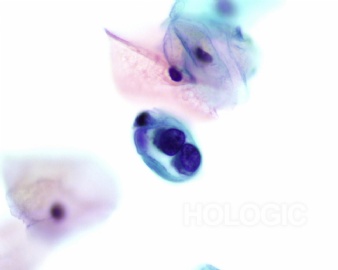
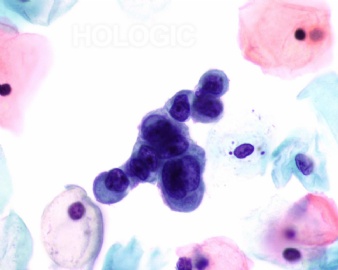
On cytology the cells occur as isolated cells or in small groups. The cells have eccentric, large nuclei and can have one or multiple prominent nucleoli. The amount of cytoplasm can vary and is foamy and vacuolated. Occasionally signet ring forms are present. The characteristic pattern shows cell within cell clusters. Cytologically, it is not possible to distinguish between the cells of Paget's disease and an underlying invasive adenocarcinoma.
Histology:
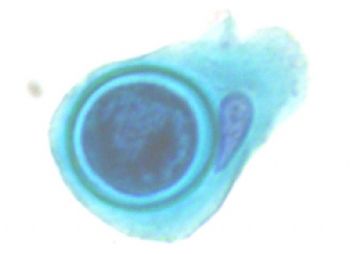
Histologically the cells of Paget's disease are large and pale, occurring both isolated or in aggregates in the epidermis. Signet ring shapes can be found. The cytoplasm is mucicarmine positive. There may be invasion of the dermis and involvement of the hair follicles, pilosebaceous units, sweat ducts and sweat glands.
Prognosis and Treatment:
The treatment of Paget's disease of the vulva is dependant on the extent of epidermal involvement and whether invasive carcinoma is present. Because the cells have a large horizontal spread into grossly normal appearing skin, there are frequent recurrences. Simple vulvectomy with a wide excision is the treatment of choice. Radiation is of no value because of the diffuse nature of the disease. Since repeated excisions are often not successful, topical chemotherapy, bleomycin and imiquimod, have been attempted with some success. It is rare for intraepithelial Paget's to progress to invasive carcinoma; however, it has been documented. There is a poor prognosis in association with invasive adnexal carcinoma; therefore the recommended treatment when invasive carcinoma is present is radical vulvectomy with bilateral inguinal lymphadenectomy.
References:
1. Fu, Y. Pathology of the Uterine Cervix, Vagina, and Vulva Second Edition. 2002: 194.
2. Bibbo, M. Comprehensive Cytopathology Second Edition. 1997: 283.
3. Atkinson, B., Silverman, J. Atlas of Difficult Diagnoses in Cytopathology. 1998: 149.
4. Watring, E., Roberts, J., Lagasse, L., Berman, M., Ballon, S., Moore, J., Schlesinger, R. Treatment of Recurrent Paget's disease of the Vulva with Topical Bleomycin. Cancer 41:10-11, 1978.
5. VanDerWalt, A., VanRooyan, A., Cominos, D. Paget's disease of the Vulva. S. Afr. Medical Journal 51:206-7, 1977.
6. Hatch, K., Davis, J. Complete Resolution of Paget's Disease of the Vulva with Imiquimod Cream. Journal of the Lower Genital Tract Disease 12(2): 90-4, April 2008
本帖最后网站上的诊断是这样的;是原网作者观点;不代表本人和华夏网任何个人观点。请自由引用。(以下内容我不提供翻译;请大家自由引用和翻译——大家一起学专业和英文)
Cytologic diagnosis: Epithelial Cell Abnormalities: Carcinoma, consistent with known clinical history of Paget's disease.
Biopsy diagnosis: Bx of vulva, same day as cytology: Poorly Differentiated Adenocarcinoma with Pagetoid spread. Bx of lower vulva 5 days later: Extramammary Paget's disease and Invasive Adenocarcinoma. Vulvar excision one month later: Infiltrating Poorly Differentiated Adenocarcinoma with overlying Paget's disease
Case provided by: Long Island Jewish Medical Center Lab, New Hyde Park, NY
Etiology:
Paget's disease can be located at various sites including the nipple, eyelid, axilla, perianal region, mons pubis, glans penis, and the vulva. Paget's disease of the vulva is associated with a higher than normal incidence of other malignancies, breast cancer being the most common. Histologically all of the sites are similar; however they seem to have a different morphogenesis. Mammary Paget's disease is almost always associated with intraductal or invasive ductal carcinoma of the breast. It is thought that there is a migration of malignant cells thru both the mammary and lactiferous ducts which result in invasion of the epidermis. Compared to the vulvar type in which 70% of cases have only purely intraepidermal carcinoma with only the remaining 30% having an in situ or invasive adnexal carcinoma.
Clinical Features:
Paget's disease of the vulva has been reported in women ranging from 38-87 years of age with an average age of 67. This disease predominately affects white postmenopausal women. Chief complaints, commonly present for many years, include pruritis, irritation, a burning sensation, and localized discomfort. The most commonly affected site is the labia majora. The lesions are erythematous, eczematous and indurated. They are often ulcerated and bleed easily on contact.
Cytology:
On cytology the cells occur as isolated cells or in small groups. The cells have eccentric, large nuclei and can have one or multiple prominent nucleoli. The amount of cytoplasm can vary and is foamy and vacuolated. Occasionally signet ring forms are present. The characteristic pattern shows cell within cell clusters. Cytologically, it is not possible to distinguish between the cells of Paget's disease and an underlying invasive adenocarcinoma.
Histology:
Histologically the cells of Paget's disease are large and pale, occurring both isolated or in aggregates in the epidermis. Signet ring shapes can be found. The cytoplasm is mucicarmine positive. There may be invasion of the dermis and involvement of the hair follicles, pilosebaceous units, sweat ducts and sweat glands.
Prognosis and Treatment:
The treatment of Paget's disease of the vulva is dependant on the extent of epidermal involvement and whether invasive carcinoma is present. Because the cells have a large horizontal spread into grossly normal appearing skin, there are frequent recurrences. Simple vulvectomy with a wide excision is the treatment of choice. Radiation is of no value because of the diffuse nature of the disease. Since repeated excisions are often not successful, topical chemotherapy, bleomycin and imiquimod, have been attempted with some success. It is rare for intraepithelial Paget's to progress to invasive carcinoma; however, it has been documented. There is a poor prognosis in association with invasive adnexal carcinoma; therefore the recommended treatment when invasive carcinoma is present is radical vulvectomy with bilateral inguinal lymphadenectomy.
References:
1. Fu, Y. Pathology of the Uterine Cervix, Vagina, and Vulva Second Edition. 2002: 194.
2. Bibbo, M. Comprehensive Cytopathology Second Edition. 1997: 283.
3. Atkinson, B., Silverman, J. Atlas of Difficult Diagnoses in Cytopathology. 1998: 149.
4. Watring, E., Roberts, J., Lagasse, L., Berman, M., Ballon, S., Moore, J., Schlesinger, R. Treatment of Recurrent Paget's disease of the Vulva with Topical Bleomycin. Cancer 41:10-11, 1978.
5. VanDerWalt, A., VanRooyan, A., Cominos, D. Paget's disease of the Vulva. S. Afr. Medical Journal 51:206-7, 1977.
6. Hatch, K., Davis, J. Complete Resolution of Paget's Disease of the Vulva with Imiquimod Cream. Journal of the Lower Genital Tract Disease 12(2): 90-4, April 2008