| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
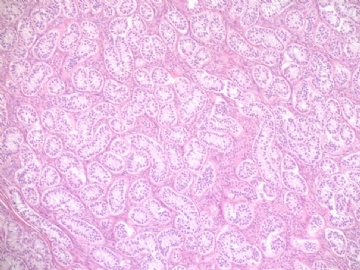
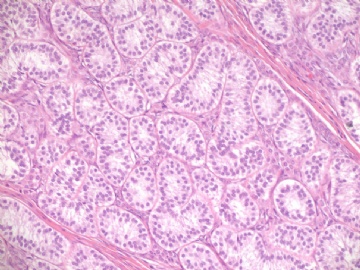
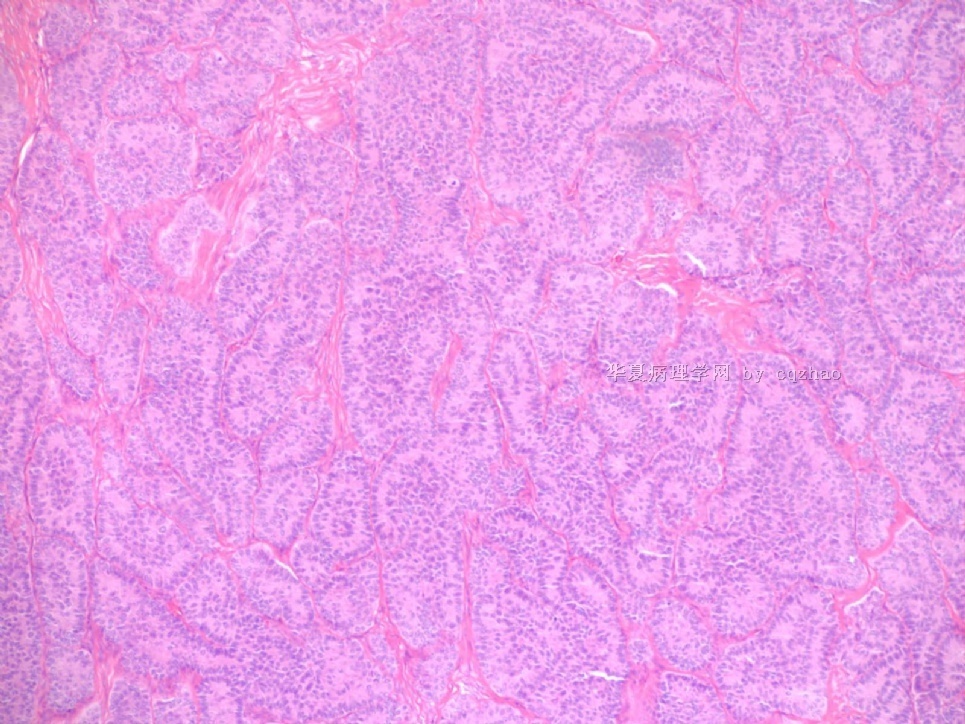
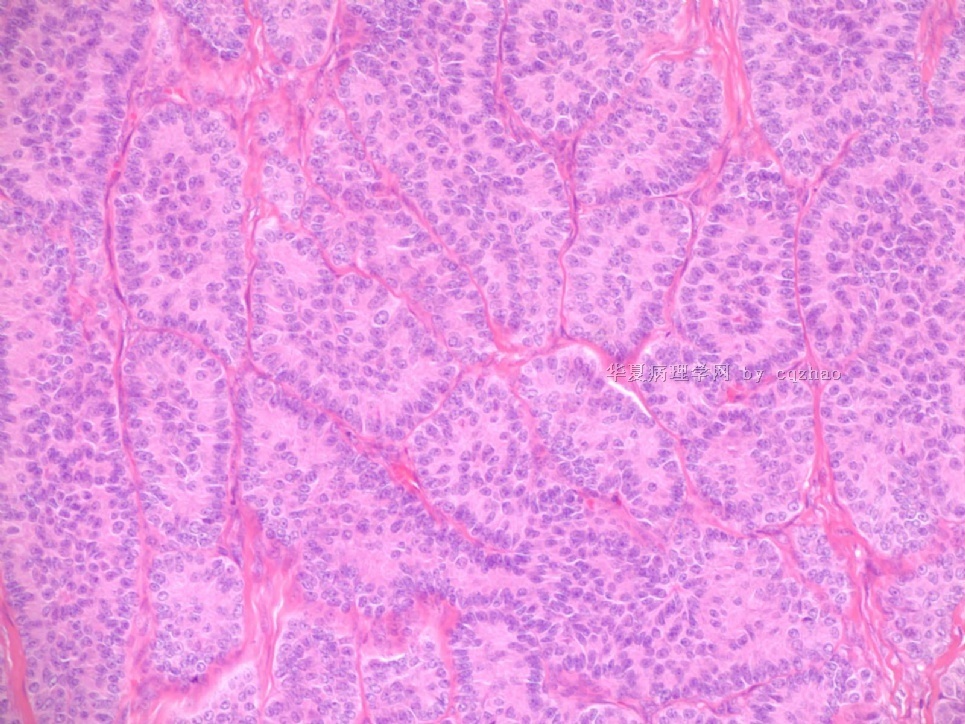
- Sharing some photos of ovarian pure sertoli cell tumors
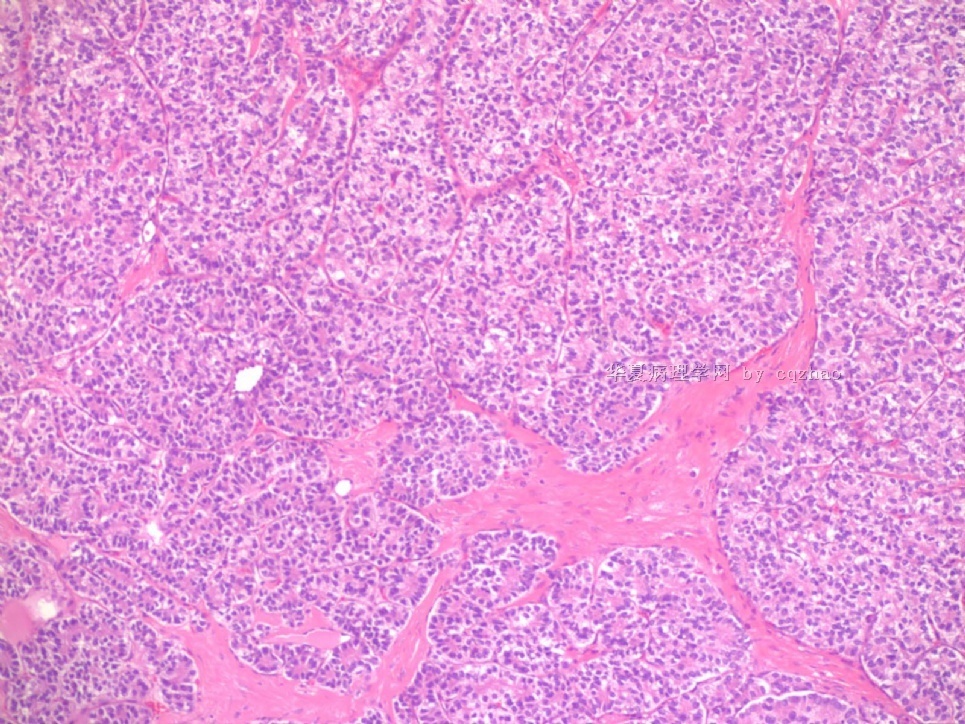
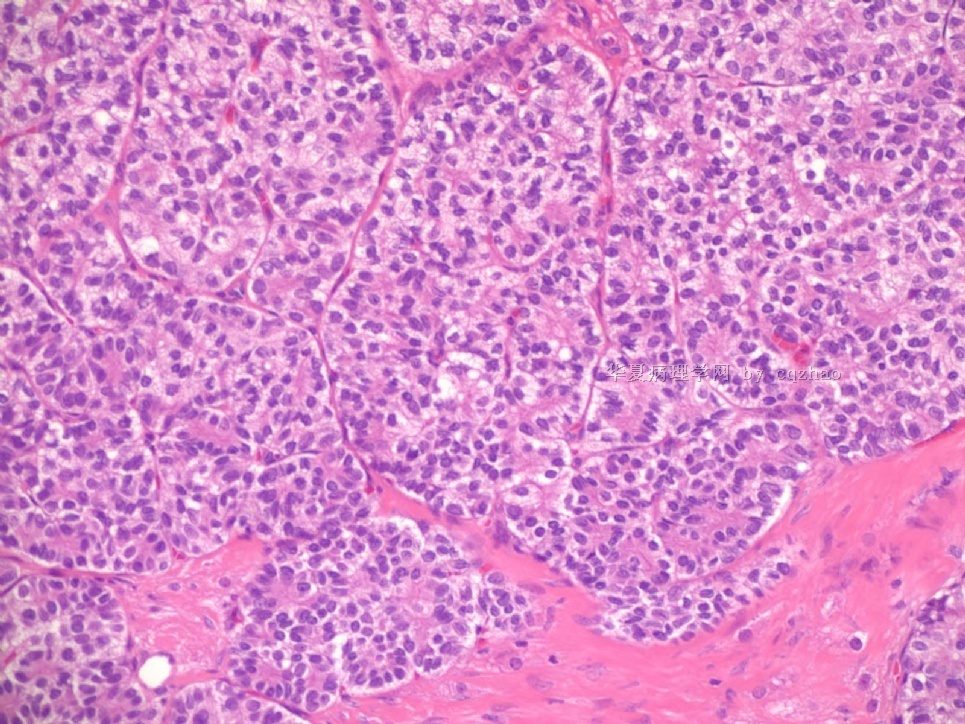
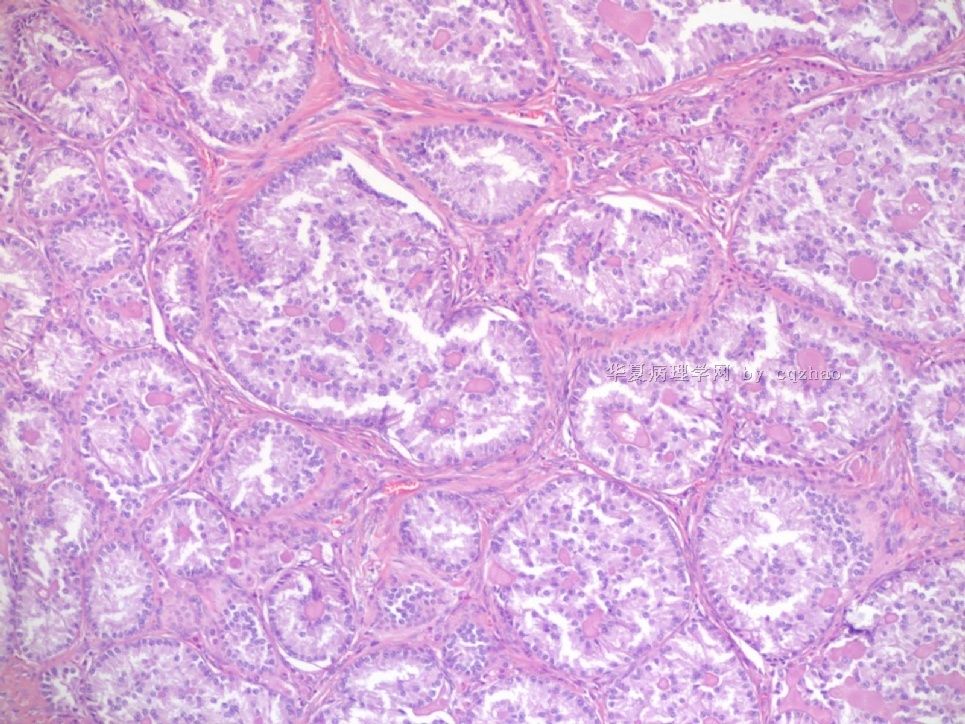
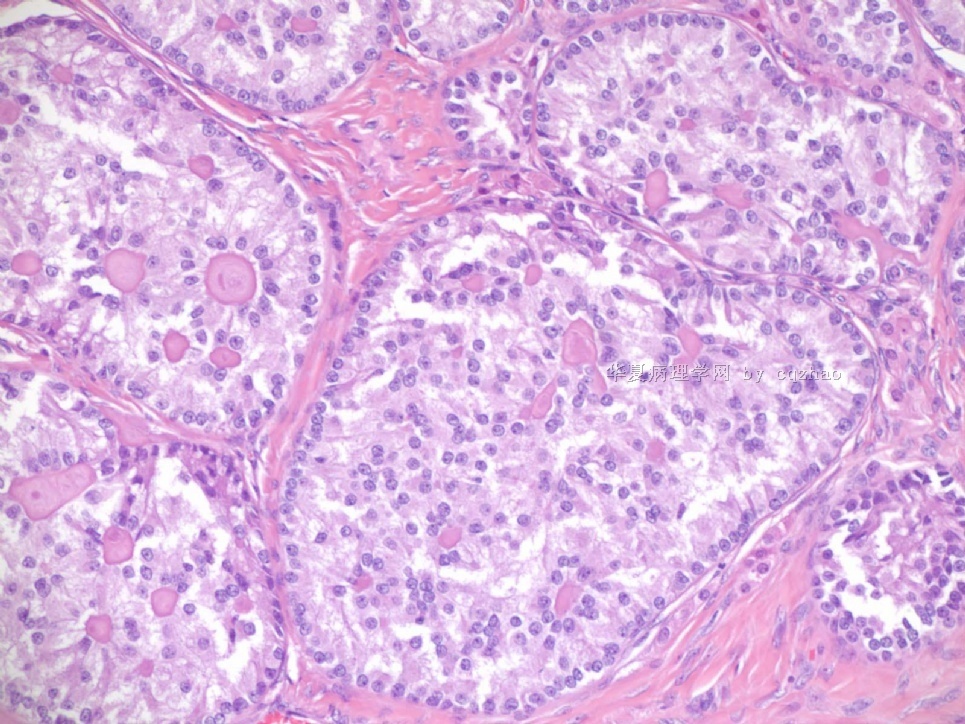
For the last case, please observe the cytomorphology and architectures of the tumor more carefully. Did you notice some compacted tubular structures? Did you see granulosa tumors like this one before?
I can tell you that all these tumors are ov sex cord tumors. Just think a little more and give the reasonable guess. Frankly speaking rare people in the world have seen this growth pattern of the tumor. Now you are one of them.
-
本帖最后由 于 2009-07-27 22:59:00 编辑
|
For the last case, please observe the cytomorphology and architectures of the tumor more carefully. Did you notice some compacted tubular structures? Did you see granulosa tumors like this one before? I can tell you that all these tumors are ov sex cord tumors. Just think a little more and give the reasonable guess. Frankly speaking rare people in the world have seen this growth pattern of the tumor. Now you are one of them. |
cqzhao老师回复:最后一例,注意仔细观察其细胞形态和肿瘤结构。看到那些比较紧密的管状结构了吗?以前看到过这样的粒层细胞瘤吗?
可以告诉大家的是,这几个病例都是卵巢的性索细胞肿瘤。仔细考虑一下,给出reasonable guess。老实说,看到具有这样的生长方式的这种肿瘤的人不多 (the fifth case)。现在你们就是其中之一……

- 赚点散碎银子养家,乐呵呵的穿衣吃饭
-
本帖最后由 城北 于 2017-02-25 10:18:06 编辑
All of them are pure sertoli cell tumors (SCT) from AFIP files I once used them for IHC study (about 20 stains for each cases). I reviewed 150 cases of pure SCT and used 40 cases for IHC study at AFIP.
As some of you mentioned the case 4 may be called sex cord tumor with annular tubules (SCTAT). Some people may call SCT, complex tubular pattern (Tavassoli). Basically they are the same tumors called different tumors by different authours. People though SCTAT may be related with Peutz-Jeghers syndroma (P-Z-S). In fact Dr. Young paper indicated 11% (6/54)of SCT patients had PJS.
Case 5 is SCT with spindle cell growth pattern. You will appreciate the tubular structure if you see the photos carefully.
Dr. Young paper: Among 54 SCT, The predominant microscopic pattern was tubular, seen, albeit often only focally, in all tumors; other patterns were cords or trabeculae (28), diffuse (21), pseudopapillary (4), retiform (3), islands or alveolar arrangements (3), and spindled (3). The tubules were solid or hollow with the former being somewhat more common.
Remeber that tubular structures are present in all SCT even though they can be very focal.
The largest and best paper about morphogolgic description and clinical followup results of SCT is Dr Young's paper.
The largest and detailed IHC studies on SCT are my two papers. I paste these three papers in the following for some ones who may be interested.
-
本帖最后由 于 2009-07-28 05:37:00 编辑
-
James Wright Pathology Laboratories, Massachusetts General Hospital, Harvard Medical School, Boston, MA 02114, USA. eoliva@partners.org
Am J Surg Pathol. 2005 Feb;29(2):143-56.![]()
Sertoli cell tumors of the ovary: a clinicopathologic and immunohistochemical study of 54 cases.
Ovarian Sertoli cell tumors are rare, and their morphologic spectrum, behavior, and factors influencing the latter are not clearly established. They may be mimicked by many different tumors, some of them more frequent than Sertoli cell tumors; immunohistochemistry may aid in this differential, but its role has not been analyzed in a large series. We studied the clinicopathologic features of 54 Sertoli cell tumors, including the immunohistochemical profile of 23 of them. The patients, 6 of whom had Peutz-Jeghers syndrome, ranged from 2 to 76 years of age (mean, 30 years). Eleven patients had estrogenic and 4 had androgenic manifestations. The tumors ranged from 0.8 to 30 cm, with the majority being in the range of 4 to 12 cm. They were all unilateral, usually solid, and often yellow. The predominant microscopic pattern was tubular, seen, albeit often only focally, in all tumors; other patterns were cords or trabeculae (28), diffuse (21), pseudopapillary (4), retiform (3), islands or alveolar arrangements (3), and spindled (3). The tubules were solid or hollow with the former being somewhat more common. Delicate septa were occasionally seen and were conspicuous in areas of one tumor. The stroma was abundant in 15 tumors with marked sclerosis in 4. The cells usually had pale to occasionally densely eosinophilic cytoplasm, but 6 tumors were composed of cells with prominent foamy cytoplasm, falling in the category of "lipid-rich" Sertoli cell tumor, and one had cells with clear non-foamy cytoplasm. Forty-four tumors were stage I (42 of them were stage Ia and 2 were stage Ic), 1 was stage II, 3 were stage III, and 6 were not adequately staged. Follow-up was available for 27 patients with stage I tumors, and all were alive and well at last follow-up except for 2 patients with stage Ia and 1 with stage Ic disease. Those 3 patients had pelvic-abdominal recurrences 18, 36, and 9 months, respectively, after the initial diagnosis. Two of the three clinically malignant stage I tumors had moderate to severe cytologic atypia and brisk mitotic activity (>5 or more mitoses/10 high power fields [HPFs]), and one of these had tumor cell necrosis. Among the 10 clinically benign stage I tumors with more than 5 years of follow-up, only 3 had >5 mitoses/10 HPFs, but none had more than mild cytologic atypia and none had tumor cell necrosis. Two of the three patients with stage III disease had follow-up information and one was alive at 16 months and the second developed splenic metastases 2 years after the initial diagnosis. Two of the three stage III tumors had at least moderate cytologic atypia and brisk mitotic activity. Immunohistochemical stains showed positivity for AE1/3-Cam5.2 in 15 of 23 tumors; Epithelial membrane antigen (EMA) was negative in all the tumors. Inhibin was positive in 18 of 22 tumors, calretinin in 10 of 20, CD99 in 19 of 22, vimentin in 17 of 18, smooth muscle actin in 4 of 18, neuron specific enolase in 8 of 16, S-100 in 2 of 20, and chromogranin was negative in all 21 cases studied. Although Sertoli cell tumors usually have a distinctive tubular pattern that facilitates the diagnosis, other patterns may occasionally predominate, causing confusion with various other primary and metastatic ovarian tumors. EMA, inhibin, and chromogranin represent the most helpful triad of immunomarkers serving to exclude two common mimics of Sertoli cell tumors (endometrioid carcinoma [inhibin-; EMA+; chromogranin-] and carcinoid tumor [inhibin-; EMA+; chromogranin+]). Although CD99 and calretinin are often expressed in these tumors, they are much less specific and not as helpful in the differential diagnosis. Most Sertoli cell tumors are stage I, unilateral, cytologically bland, and clinically benign, but occasional examples are high stage, and about 11% of stage I tumors have worrisome histologic features that may portend an adverse outcome. The tumors typically occur in young females, sometimes children who typically present with sexual precocity, and occasional patients have Peutz-Jeghers syndrome.
-
Am J Surg Pathol. 2007 Feb;31(2):255-66.
-
Comparative analysis of alternative and traditional immunohistochemical markers for the distinction of ovarian sertoli cell tumor from endometrioid tumors and carcinoid tumor: A study of 160 cases.
Department of Gynecologic and Breast Pathology, Armed Forces Institute of Pathology, Washington, DC, USA. chengquanzhao@yahoo.com
The main neoplasms in the differential diagnosis for primary ovarian tumors with a tubule-rich pattern are pure Sertoli cell tumor, endometrioid tumors (including borderline tumor, well-differentiated carcinoma, and the sertoliform variant of endometrioid carcinoma), and carcinoid tumor. Because traditional immunohistochemical markers [pan-cytokeratin (pan-CK), low molecular weight cytokeratin (CK8/18), epithelial membrane antigen (EMA), inhibin, calretinin, CD99, chromogranin, and synaptophysin] can occasionally have diagnostic limitations, the goal of this study was to determine whether or not any alternative markers [cytokeratin 7 (CK7), estrogen receptor (ER), progesterone receptor (PR), CD10, and CD56] have better diagnostic utility when compared with traditional markers for this differential diagnosis. Immunohistochemical stains for alternative, as well as traditional, markers were performed on the following primary ovarian tumors: pure Sertoli cell tumor (n = 40), endometrioid borderline tumor (n = 38), sertoliform endometrioid carcinoma (n = 13), well-differentiated endometrioid carcinoma (n = 27), and carcinoid tumor (n = 42). Extent and intensity of immunostaining were semiquantitatively scored. In addition, immunohistochemical composite scores (ICSs) in positive cases were calculated on the basis of the combination of extent and intensity scores. Cytokeratin 7 (CK7) was positive in 97% of endometrioid tumors, 13% of Sertoli cell tumors, and 24% of carcinoid tumors. The differences in the mean ICSs for endometrioid tumors versus Sertoli cell tumor or carcinoid tumor were statistically significant (P values ranging from <0.001 to 0.018). ER and PR were positive in 87% and 86% of endometrioid tumors, 8% and 13% of Sertoli cell tumors, and 2% each of carcinoid tumors, respectively. The differences in the mean ICSs for endometrioid tumors versus Sertoli cell tumor were statistically significant (P values ranging from <0.001 to 0.012). Among the epithelial markers, EMA seemed to be the most discriminatory but only slightly better than CK7, ER, or PR. Pan-CK and CK8/18 were not helpful. CD10 showed overlapping patterns of expression in all categories of tumors. Among the sex cord markers, CD10 was markedly less useful than inhibin or calretinin; CD99 was not discriminatory. CD56 showed overlapping patterns of expression in all categories of tumors. Among the neuroendocrine markers, CD56 was less useful than chromogranin or synaptophysin. When traditional immunohistochemical markers are problematic for the differential diagnosis of ovarian Sertoli cell tumor versus endometrioid tumors versus carcinoid tumor, adding CK7, ER, and/or PR to a panel of markers can be helpful. Endometrioid tumors more frequently express CK7, ER, and PR and show a greater extent of immunostaining in contrast to Sertoli cell tumor and carcinoid tumor. Compared with traditional epithelial markers, CK7, ER, and PR are nearly as advantageous as EMA. Inhibin is the most discriminatory sex cord marker, and CD10 is not helpful in the differential diagnosis. Chromogranin and synaptophysin are excellent discriminatory markers for carcinoid tumor, and CD56 is neither sufficiently sensitive nor specific enough for this differential diagnosis to warrant its use in routine practice.