| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- 放疗后乳房(cutaneous)高级别血管肉瘤(cqz-23)
A few words for post radiation angiosarcona (AS)
1. The interval between radiation and AS is from 3 y to 12 y, mostly within 6 y.
2. Cutaneous presentation is more often than parenchynal AS.
3. Women with primary AS presentd with metastasis more often those with postradiaton AS.
4. Overall survival rates were no significantly different between primary and postradiation AS.
5. More cases are lymphatic origin in my impression. Correct me if it is wrong.
6. Histologic features of postradiation AS may be different from primary AS. You can find some papers to read for details if you are interested. I do not think it is very important for our dx. We need to consider the lesions and need some IHC.
Thank all of you for the discussion.
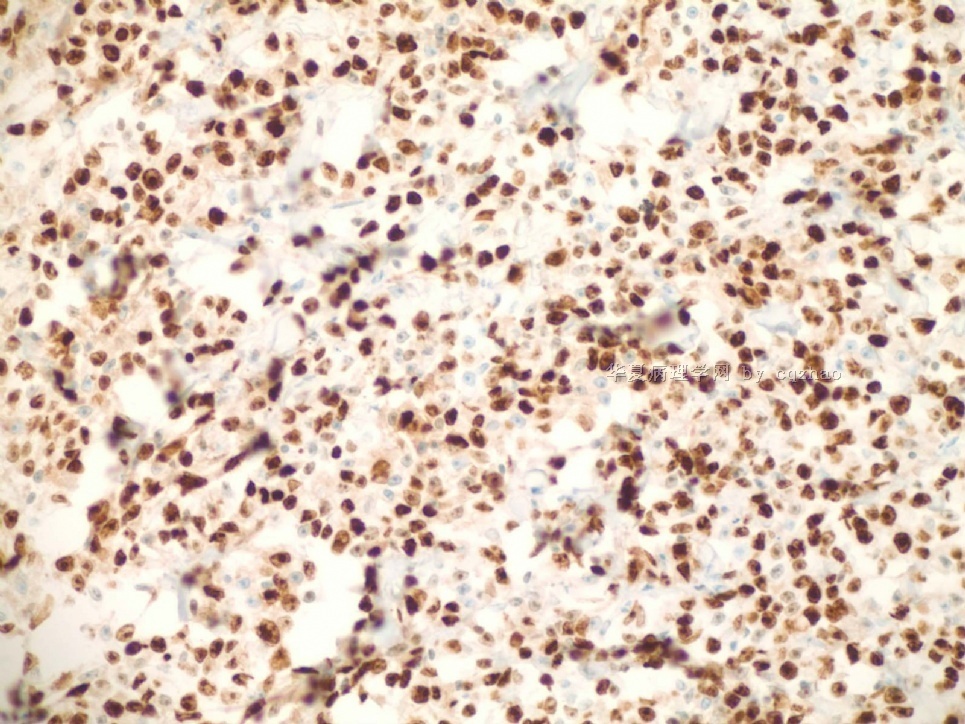
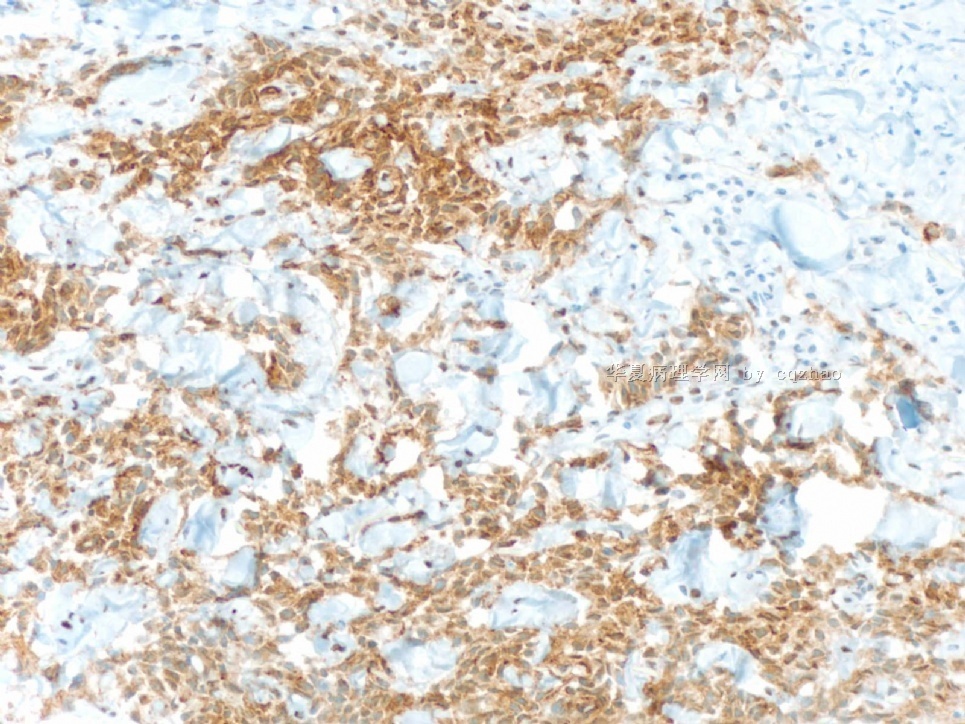
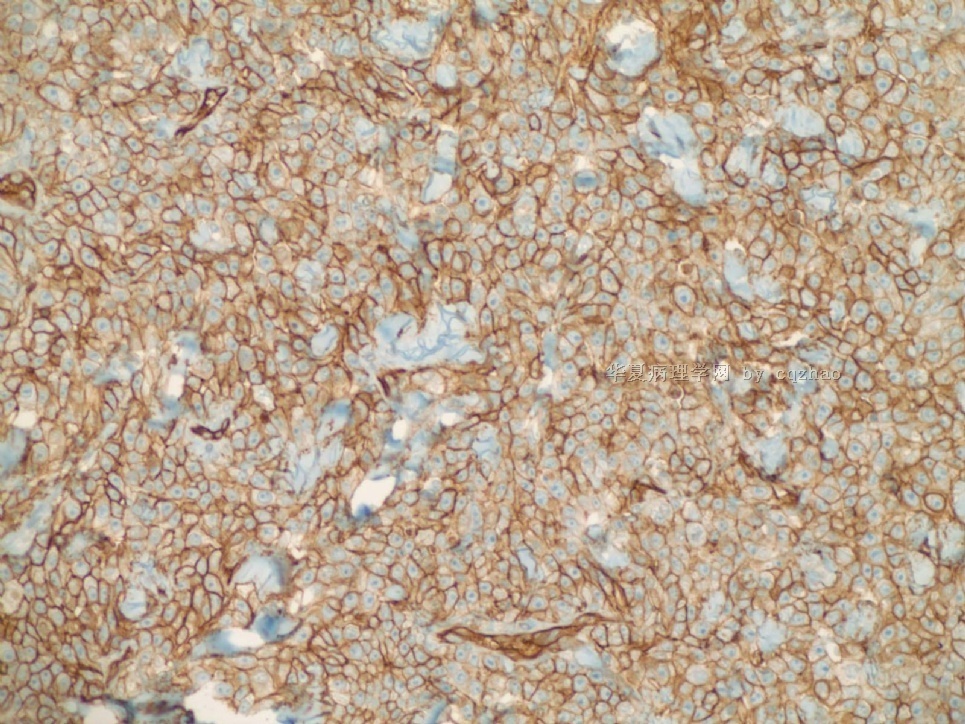
Just feel interested about ki67 proliferative index in high grade angiosarcoma. I did a ki67 stain for the purpose of education (not charge patient due to no meaning for dx). You can see the tumors are diffusely positive for ki67. I also asked the lab to do a D2-40 stain for education. We will not charge patients if the stains are for education. Also we will not report these results in the pathology reports.
D2-40 stain is positive for lymphatic endothelieum.
-
本帖最后由 于 2009-07-26 08:22:00 编辑
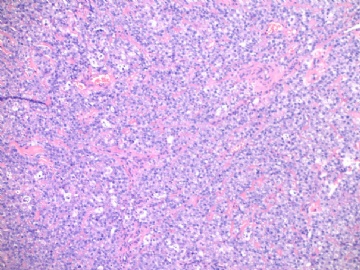
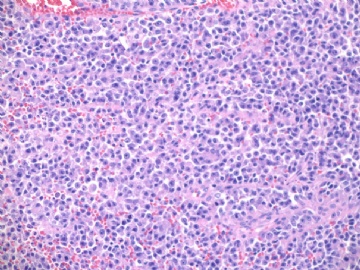
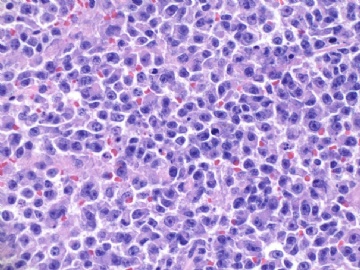
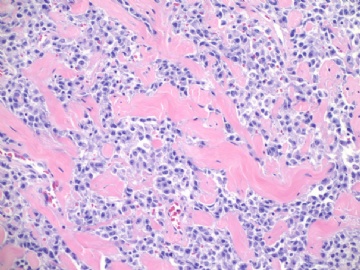
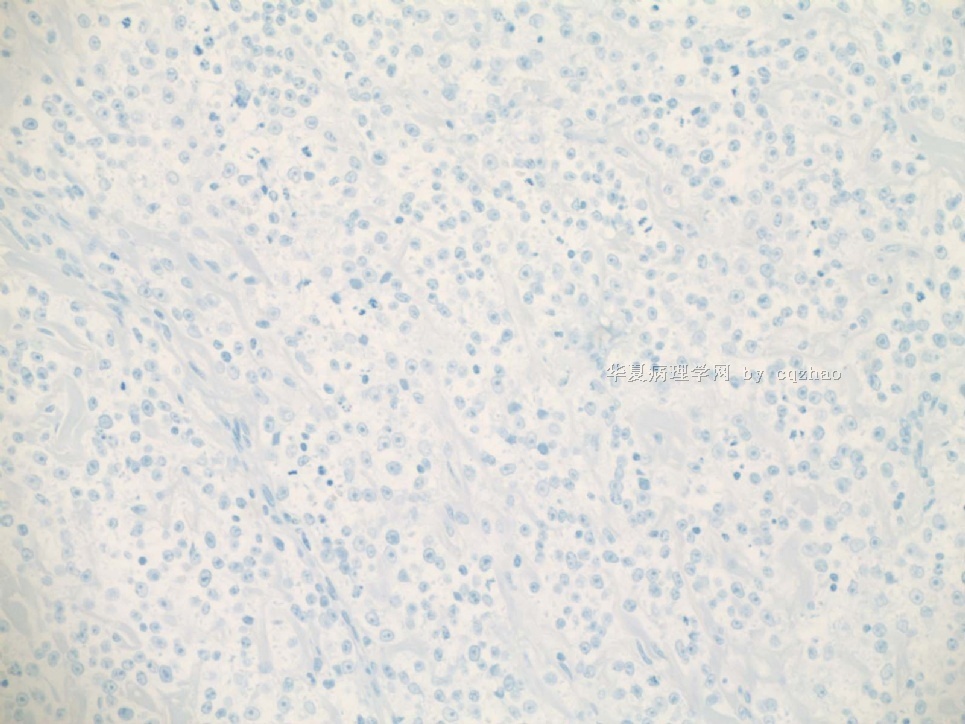
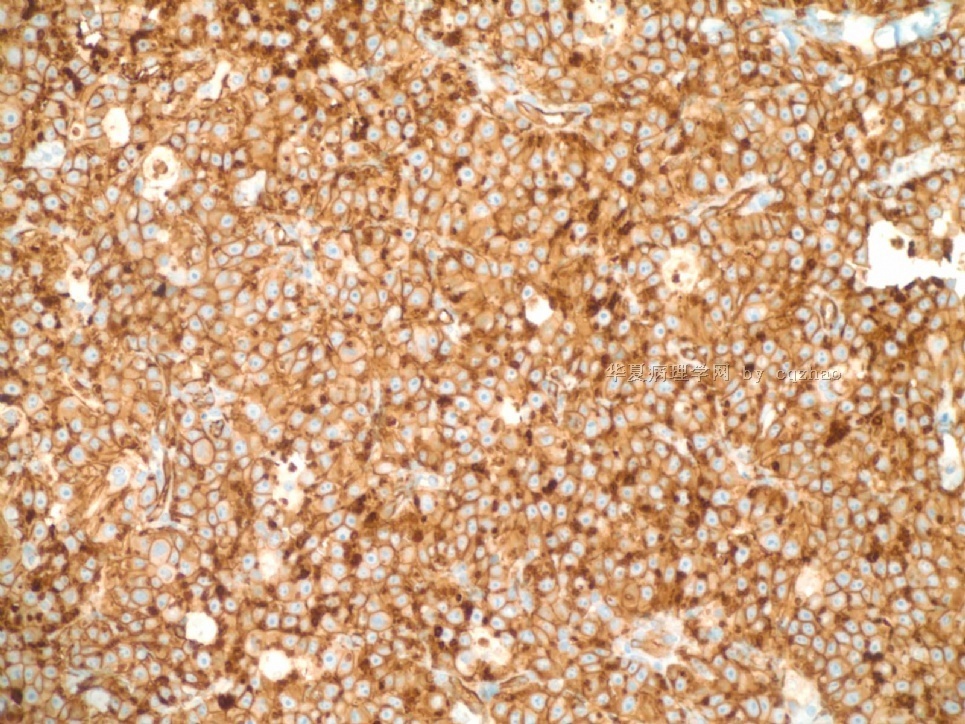
This biopsy speciment was diagnosed as high grade angiosarcoma and the pt had mastectomy. Paste here some photos from mastecetomy. I want to show you the high grade angiosarcoma often mixed with low grade component.
The cytologic features of the tumor cells between low grade and high grade solide areas are similar.
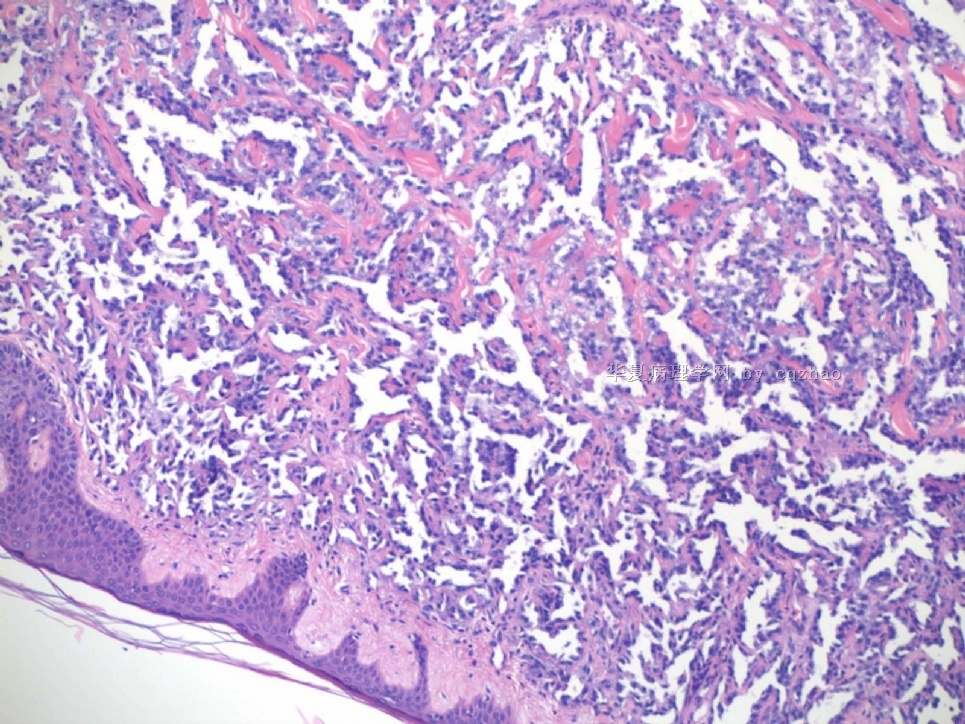
名称:图1
描述:图1
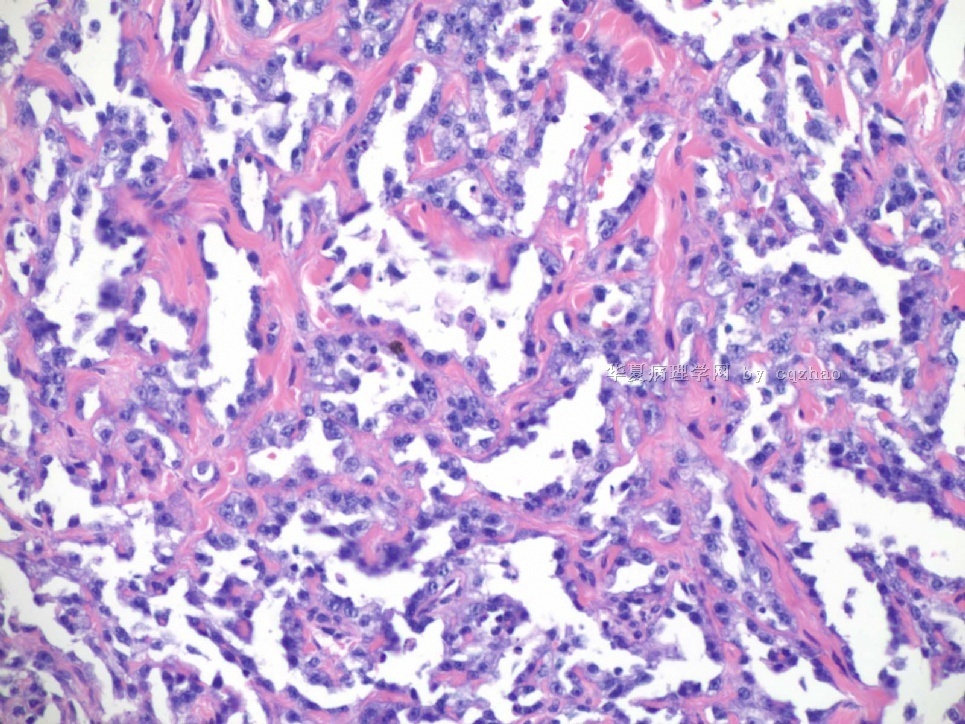
名称:图2
描述:图2
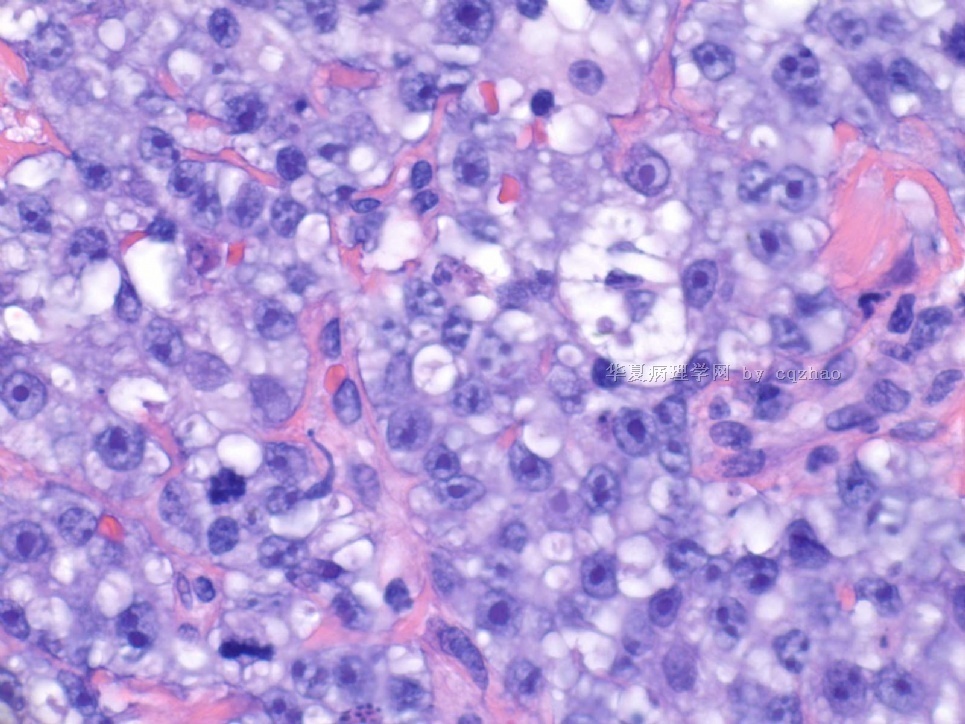
名称:图3
描述:图3
| 以下是引用wq_9603在2009-7-13 7:14:00的发言:
图2、3中红细胞浸润 有无提示意义? |
Good observation.
Clearly you can appreciate RBC in fig 2 and 3, plus pt's hx of breast ca with segmental mastectomy, radiation, chemotherapy. Also remember the time perioid is about six years (2003-2009).
Of cause we need IHC for this case. However, what lesion will be your first differential dx?
-
本帖最后由 于 2009-07-14 21:03:00 编辑
Good analysis.
It is unfair. I should tell you the history.
The patient had invasive ductal carcinoma with segmental mastectomy. She then received radiation and chemotherapy.
Now what are your differential dx and IHC?
abin译:
分析得好。
不公平,我应该为你们提供病史。
患者有浸润性导管癌并做过乳腺区段切除,然后接收了放疗和化疗。
现在你的鉴别诊断是IHC?