| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- Acute renal failure after endocarditis.
| 姓 名: | ××× | 性别: | Male | 年龄: | adult |
| 标本名称: | |||||
| 简要病史: | Patient was hospitalized for endocarditis, and then developed acute renal failure. | ||||
| 肉眼检查: | |||||
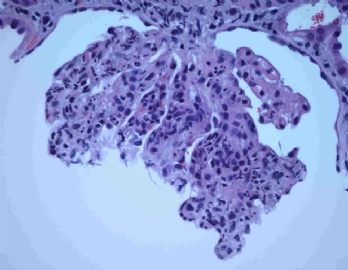
Hi, I like the translation 白金耳样结构 (wire loop). Is there anyone who calls it as 烧红的白金耳样结构?
"Wire loop" is usually seen in lupus nephritis. If I recall correctly, I also saw it once in a case of membranoproliferative glomerulonephritis (MPGN).
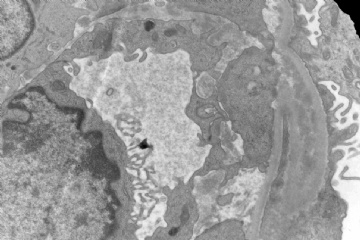
The nature of this lesion is dense, confluent subendothelial deposition which is so large that we can see it at light level. Theoretically, it should be seen in any immune complex GN with large subendothelial deposits. In real life, we almost exclusively see it in lupus nephritis, WHO class IV. But it is not pathognomonic lesion. The only true pathognomonic lesion of lupus nephritis is hematoxylin body, which is only seen in less than 2% of the biopsy.
I agree with your hypothesis that in the above case, wire loop 是因为细菌性心内膜炎导致免疫复合物沉积的过多引起的. It is unfortunate that it is so focal that I could not demonstrate it in the EM material.
Hi, 小荷 : It seems that nephropathology is 阳春白雪 among all pathologists everywhere. I am not surprised that the response is scant. Vast majority of surgical pathologists do not want to touch renal pathology. I work in a department with 11 pathologists and I am the only one doing renal pathology. Once I am on vacation, all renal biopsies will be shipped to other medical center for coverage. We need someone to write a book titled as "Nephropathology for General Surgical Pathologists", to attract more pathologists to this field.
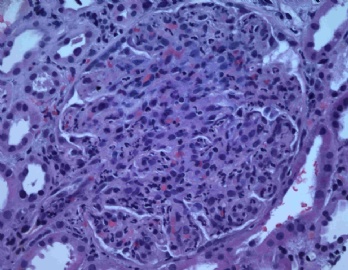
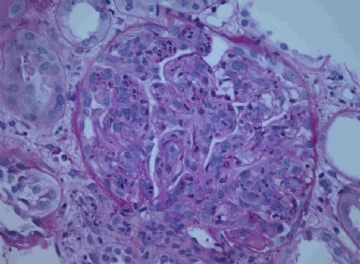
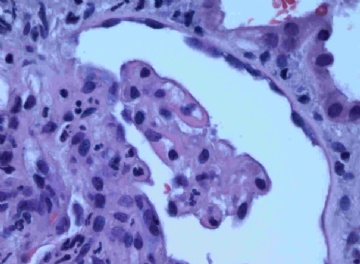
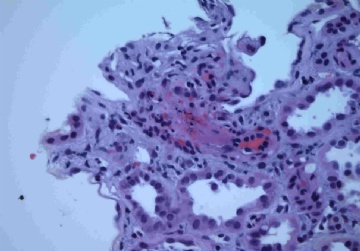
Let us go back the above case, which I signed out as infectious endocarditis glomerulonephritis. On the light level, there are many neutrophils infiltrating the glomerulus. So the morphological diagnosis is acute diffuse intracapillary proliferative or exudative glomerulonephritis. It is often associated with infection. This patient has on-going infectious endocarditis, being hospitalized. The glomerulonephritis (GN) is etiologically related to infectious endocarditis. The vasculitis could be part of the process (see photo 5).
The immunofluorescence is not typical. Based on my reading, IgM is supposed to be the dominant deposition component in infectious endocarditis GN. The other sudies found that "IgG is most often and most intensely in acute postinfectious GN whereas IgM is seen most often and most intensely in GN caused by persistent infections".
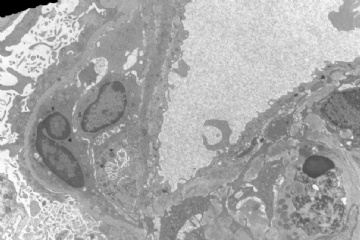
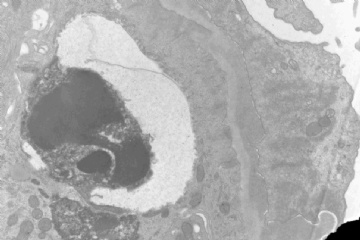
The EM shows subendothelial and subepithelial deposits. One hump like deposit is seen at the edge of the photo 8 (right lower corner).
If the pathologist is a lumper, he may call this case as acute post-infectious GN. For this case, I am the spiltter. The vasculitis (photo 5) and "wire-loop" pattern (photo 4) lead me to that conclusion. This is a rare case. I welcome colleagues' comment and critiques.