| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
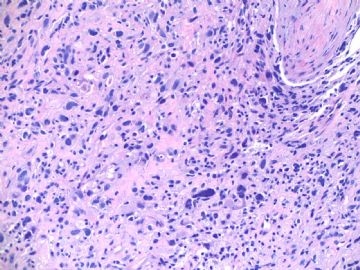
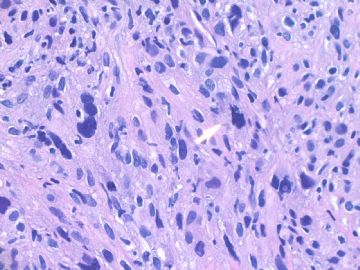
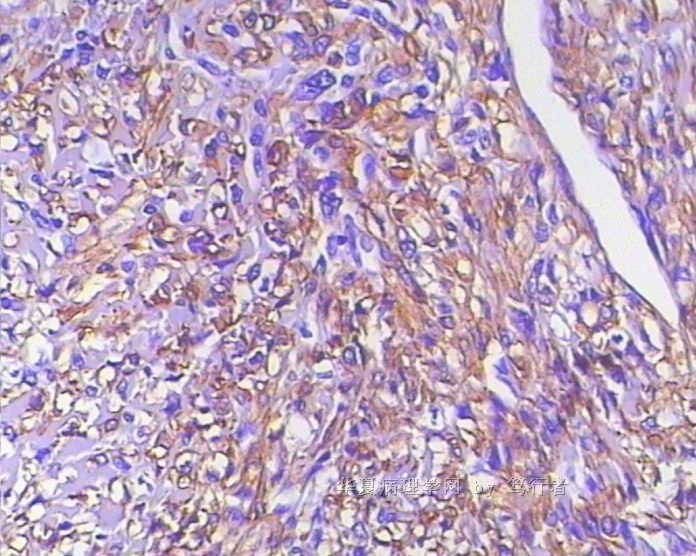
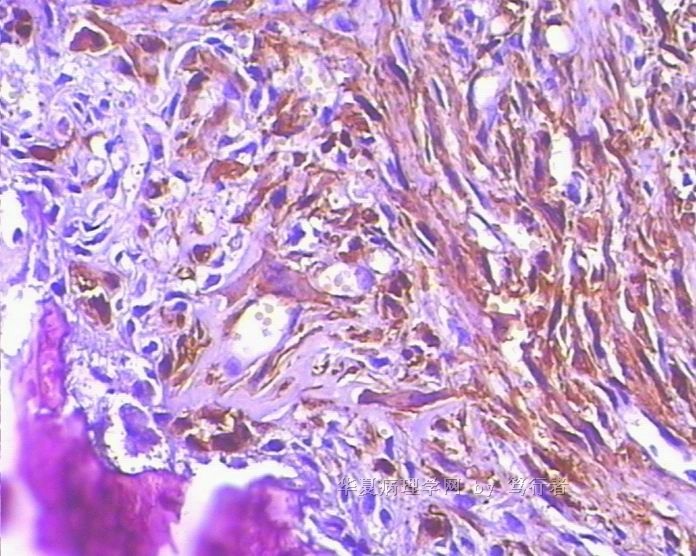
- B1803少见乳腺肿物,鉴别诊断? (cqz-18, 5-7-2009)
| 姓 名: | ××× | 性别: | 年龄: | ||
| 标本名称: | |||||
| 简要病史: | |||||
| 肉眼检查: | |||||
about 60 y/f, right breast mass 2 cm by imaging, breast core biopsy.
1. Your differential diagnosis?
2. What will you do next?
Please do not just give a diagnosis. Your dx is a guess dx even though your diagnosis may be right.
As pathologists we should learn how to analyse our cases with logic thought.We should have differential dx for all cases in our mind even for the easy cases. We can use available sources (such as IHC, molecular methods, history, consultation) to rule in or rule out the differential dx, then make the final dx.
Learning the priniciple for diagnosis is much more important than learning a few cases.
-
本帖最后由 于 2009-05-07 18:28:00 编辑
相关帖子
-
Medicina (B Aires). 2006;66(2):135-8.
-
[Primary sarcomas of the breast]
[Article in Spanish]Departamento de Anatomía Patológica, Instituto de Oncología Angel H Roffo, Facultad de Medicina, Universidad de Buenos Aires.
Primary sarcomas of the breast are extremely rare with less than 1% of all malignant tumours of the breast reported in literature. At our Institution 1315 malignant tumours of the breast were diagnosed between 1999-2004; nine of them corresponded to primary sarcomas: angiosarcoma (3), leiomyosarcoma (1), low-grade fibromyxoid sarcoma (1), dematofibrosarcoma protuberans (1), liposarcoma (1), osteosarcoma (1), malignant peripheral nerve sheath tumour (1). Histopathological specimens stained with routine techniques and immunoperoxidase were reviewed; proliferation index and p53 over-expression were also determined. Patients' clinical reports were also reviewed to determine prognosis (favorable and unfavorable). The incidence observed (0.7%) is similar to those already published by others authors. Proliferation index was correlated with type of evolution, being an unfavourable prognosis factor when it was equal or major to 30%. Most of the tumours (67%) showed p53 (mayor or equal to 20% of nuclear staining) over-expression but this did not show a direct relationship with the evolution of each neoplasm
-
Br J Cancer. 2004 Jul 19;91(2):237-41.
-
Primary breast sarcoma: clinicopathologic series from the Mayo Clinic and review of the literature.
Department of Anatomic Pathology, Pitie Salpetriere Hospital, Paris, France. camilo.adem@psl.ap-hop-paris.fr
Primary sarcomas of the breast are extremely rare, with less than 0.1% of all malignant tumours of the breast. Mayo Clinic Surgical Pathology database was searched for all breast sarcoma from 1910 to 2000. Pathology reports and slides were reviewed and tumour types were determined. Metaplastic carcinomas and phyllodes tumours were excluded. There were 25 women ranging in age 24-81 years (mean 45 years). All but one patient presented with a palpable lump. Mastectomy was performed in 19 patients and lumpectomy in five patients. Histopathological diagnoses were fibrosarcoma (six), angiosarcoma (six), pleomorphic sarcoma (six), leiomyosarcoma (two), myxofibrosarcoma (three), hemangiopericytoma (one) and osteosarcoma (one). Tumour size ranged from 0.3 to 12 cm (mean 5.7). Low-grade lesions were observed in 10 cases and high-grade in 15. Overall, mean follow-up was 10.5 years. Local recurrence was observed in 11 patients and ranged from 2 to 36 months (mean 15 m), while distant metastasis was observed in 10 patients (40%) affecting lungs, bones, liver, spleen, and skin. Of the 25 patients, 12 have died of disease and six of other causes. Five-year overall (OS) and cause-specific survival (CSS) were 66 and 70%, respectively. OS and DFS at 5 years were 91% for tumours < or =5 cm and 50% for tumours >5 cm. Tumour size was significantly associated with OS (risk ratio=1.3 per 1 cm increase; 95% CI, 1.02-1.7; P=0.036). There was no significant difference in OS or CSS between low- and high-grade lesions. In this series, tumour size was a more valuable prognostic factor than tumour grade
-
Cancer Genet Cytogenet. 2004 Feb;149(1):53-7.
-
Leiomyosarcoma of the breast: a pathologic and comparative genomic hybridization study of two cases.
Department of Pediatrics, University of Oklahoma Health Sciences Center, Oklahoma City, OK, USA.
Leiomyosarcoma is an extremely rare form of primary breast sarcoma. We present the pathologic and genetic findings of two cases of leiomyosarcoma of the breast. The patients were 44 and 52 years of age and they presented with circumscribed masses of 3.0 and 4.5 cm, (greatest dimension) respectively. Microscopically, the two tumors showed diffuse proliferation of spindle cells with oval and blunt-ended nuclei arranged in short fascicles or bundles. There was moderate cytologic atypia in both cases, and 6 and 12 mitotic figures per 10 high power fields, respectively. No epithelial component was identified. The tumor cells were strongly immunoreactive for markers of smooth-muscle differentiation, including desmin, muscle-specific actin, and smooth-muscle actin. Comparative genomic hybridization analysis showed losses of 10q (two of two cases), 13q (two of two cases), 17p (one of two cases), and gains of 1q (one of two cases) and 17p (one of two cases). The patterns of chromosomal imbalances identified in leiomyosarcoma of the breast are similar to those reported in leiomyosarcoma of soft tissue and uterus and are different from those reported for leiomyoma, indicating that these alterations may be important for development of malignant smooth-muscle tumors regardless of site or organ of origin.
-
Breast. 2001 Dec;10(6):530-4.
-
Primary leiomyosarcoma of the breast: diagnosis, management and outcome. A report of a new case and review of literature.
The Breast Surgery Unit, Belfast City Hospital, Lisburn Road, Belfast BT9 7AB, UK.
Primary leiomyosarcoma of the breast is very rare and represents a diagnostic challenge. Only 16 cases have been reported in the English language literature. We report another new case and have analysed reports of the previous cases aiming to present a simple evidence-based approach to the clinical, radiological and pathological diagnosis of this rare tumour. The average age of presentation is 56 years. All neoplasms have been limited to the breast at the time of diagnosis. The usual presentation is a slowly growing mass, but in the current case report the patient present with mastalgia. There is always a possibility of local recurrence or distant spread, which can occur many years after primary surgery. Leiomyosarcoma must be histologically distinguished from leiomyoma and the presence of >3 mitoses per 10 high-power fields is usually indicative of malignancy. Immunohistochemistry is helpful to confirm diagnosis. As this is a slow-growing malignant tumour with a propensity for local recurrence, total mastectomy is the treatment of choice. The tumour is not hormone-dependent and hormone manipulation is not a treatment option.
-
West Indian Med J. 2007 Dec;56(6):555-7.
-
Primary leiomyosarcoma of the tibia--five years without recidivism.
Orthopaedic Clinical Hospital, Lovran, Croatia. branko.sestan1@ri.htnet.hr
Primary leiomyosarcoma of the bone is a rare malignancy. Clinical follow-up suggests that primary osseous leiomyosarcoma has an aggressive biologic behaviour with poor survival time. We report a case of primary leiomyosarcoma arising from the proximal metaphysis of the right tibia of a 55-year old woman with a long follow-up period, without recidivism. Primary leiomyosarcoma has to be considered as a differential diagnostic possibility in the case of bone tumours seen on routine initial plain radiographs as lytic lesions. If the tumour has been adequately excised at the time of diagnosis, as in the present case, with adjuvant therapy protocol, the long-term prognosis of such an aggressive tumour can be exceptionally good
-
Clin Imaging. 2008 Jul-Aug;32(4):321-5.
-
Primary leiomyosarcoma of bone: a report on three patients.
Department of Orthopaedic Surgery and Traumatology, Fatih University, Alparslan Turkes Caddesi No. 57, 06510 Emek/Ankara, Turkey. atalarhakan@yahoo.com
Primary leiomyosarcoma of bone is a rare aggressive tumor that occurs mainly in older people. It resembles other malignancies clinically and radiologically, and differential diagnosis is based on histopathology, including immunohistochemistry. If leiomyosarcoma is found in bone, the possibility that it is a metastasis from a distant tumor should be investigated. The treatment is surgical excision with wide margins. Here we present three patients who had primary leiomyosarcoma of radius, ilium, and femur, respectively, and who were treated surgically
-
Sarcoma. 2002;6(1):47-50.
-
Leiomyosarcoma of bone arising in association with a bone infarct.
Department of Pathology Nuffield Department of Orthopaedic Surgery University of Oxford Nuffield Orthopaedic Centre Oxford OX3 7LD UK.
Both primary leiomyosarcoma of bone and sarcoma arising in association with a bone infarct are rare events. In this case report we describe for the first time a case of leiomyosarcoma arising in a bone infarct. The tumour arose in a medullary infarct in the proximal femur of an elderly patient. As in other cases of sarcoma arising in a bone infarct, the prognosis was poor, the patient dying within 6 months of diagnosis.
-
Cancer. 2007 Dec 25;111(6):491-8.
-
Fine-needle aspiration biopsy of high-grade sarcoma: a report of 107 cases.
Department of Pathology, The Ohio State University College of Medicine, Columbus, Ohio 4320, USA.
BACKGROUND: To the authors' knowledge, few studies exist demonstrating the reliability of fine-needle aspiration (FNA) biopsy for high-grade sarcoma (HGS). METHODS: In the current study, the authors reviewed their cytopathology database (March 2001 through January 2007) and identified all FNA cases diagnosed as HGS. They also searched their tissue database for all HGS cases that had prior FNA biopsy findings. RESULTS: A total of 107 FNA samples from 98 patients (age range, 13-90 years, with a male:female ratio of 1:1) had an FNA diagnosis of HGS, or had HGS and a prior FNA diagnosis of another entity. Ten cases were nondiagnostic. Of the 97 remaining samples, 6 were diagnosed as something other than HGS (sensitivity of 94%). The positive predictive value of an FNA diagnosis of HGS was 97% (88 of 91 cases). Fifty-four cases were diagnosed as HGS, not otherwise specified, 8 as myxofibrosarcoma, 8 as osteosarcoma, 5 as malignant peripheral nerve sheath tumor, 5 as leiomyosarcoma, 4 as Ewing sarcoma, 4 as liposarcoma, 2 as epithelioid sarcoma, and 1 as angiosarcoma. Approximately 71% of patients presented with a primary tumor, 23% with disease recurrence, and 7% with metastasis. Sites of disease included the lower extremity (59%), upper extremity (19%), trunk (15%), groin (4%), and head and neck (4%). FNA diagnosis was confirmed histologically in 88% of cases, clinically in 7% of cases, and cytogenetically in 1% of cases; 3% of cases had false-positive results and 1 patient was lost to follow-up. Sixteen of 19 patients received neoadjuvant chemotherapy based on the FNA diagnosis alone. CONCLUSIONS: A cytopathologic diagnosis of HGS was found to be accurate in 88 of 97 cases (91%) with follow-up. A FNA biopsy diagnosis of HGS appears to be clinically reliable in a high percentage of cases when used in close conjunction with the orthopedic team.
-
J Orthop Sci. 2002;7(2):267-73.
-
Primary leiomyosarcoma of the femur.
Department of Orthopaedic Surgery, Faculty of Medicine, The University of Tokyo, 7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8655, Japan.
Leiomyosarcoma usually arises in the uterus, gastrointestinal tract, retroperitoneum, or soft tissue. Primary leiomyosarcoma of bone is rare. We encountered two patients with primary leiomyosarcoma of the femur; one was a 24-year-old woman and the other, a 41-year-old woman. Bone destruction observed on plain radiographs was minimal in both patients. Magnetic resonance imaging (MRI) showed low signal intensity on T1-weighted images and high signal intensity on T2-weighted images, with these areas being much larger than the findings to be expected from the plain radiographs. Histological examination revealed spindle-cell sarcoma, with an interlacing pattern, acidophilic cytoplasm and blunt-ended or "cigar-shaped" nuclei, in both patients. In both patients, immunohistochemical examination showed positive staining for vimentin, desmin, and alpha-smooth muscle actin. Extensive examination of the gastrointestinal tract and uterus revealed no primary lesion. Therefore, the leiomyosarcoma in the femur was considered to be primary rather than metastatic. Histological examination, including immunohistochemistry, and the exclusion of an extraskeletal primary lesion, is necessary in diagnosing primary leiomyosarcoma of bone
-
Rev Chir Orthop Reparatrice Appar Mot. 2000 Feb;86(1):63-73.
-
[Primary leiomyosarcoma of bone. Report of 5 anatomo-clinical cases and review of the literature]
[Article in French]Service de chirurgie orthopédique et traumatologique B, Hôpital Cochin, 27 rue du faubourg Saint Jacques, 75014 Paris, France.
INTRODUCTION: Leiomyosarcoma is a malignant smooth muscle tumor occurring most frequently in uterus or soft tissues and more rarely in bone. MATERIALS AND METHODS: We report the clinicopathologic, immunohistochemical and ultrastructural findings of five cases of primary leiomyosarcoma of bone treated in our Department between 1991 and 1994. The pertinent medical literature is discussed. RESULTS: The tumors were located respectively in the distal tibia (n=2), the distal femur, the sternum and the ilium (n=1). Four lesions were high-grade and one low-grade. All patients (3 women and 2 men) underwent wide surgical resection associated with polychemotherapy in four cases. Two patients died of metastatic disease, two had local recurrence and one is alive with no evidence of disease at the last follow-up. DISCUSSION: Excluding cases which involve the facial skeleton, there are to our knowledge 95 cases of primary leiomyosarcoma of bone reported in the literature. This tumor arises more commonly in adults (mean age: 49 years) with an equal gender distribution and involves predominantly the long bones near the knee. In the majority of cases, plain X-rays exhibit an osteolytic lesion with cortical penetration and indistinct margins. The diagnosis is based on microscopic features demonstrating fusiform tumor cells arranged in interwoven bundles, and the immunohistochemical results of widespread cytoplasmic positivity for smooth muscle actin. The best pronostic parameter is the histologic grade correlated with both the recurrence and metastatic rates as well as the survival rate. Surgery constitutes the main treatment since chemotherapy or radiotherapy did not provide an improved prognosis over a wide resection.
-
AJR Am J Roentgenol. 1999 Mar;172(3):771-6.
-
Primary leiomyosarcoma of bone.
Department of Radiology, St. Louis University Health Sciences Center, MO 63110-0250, USA.
OBJECTIVE: This study describes radiographic and MR imaging features of primary leiomyosarcoma of bone. SUBJECTS AND METHODS: Twelve patients (five men and seven women, 39-79 years old) who were treated at two oncology centers for primary leiomyosarcoma of bone involving the femurs, tibia, ilium, and inferior pubic ramus were studied. None of the patients had preexisting disease or disease elsewhere at the time of diagnosis. Pathologic diagnosis was obtained in all patients. RESULTS: Radiographs of all patients showed a matrix that was exclusively osteolytic. In long bones (seven patients), the tumor had an average length of 11 cm (range, 7-17 cm) and revealed an elongated configuration. In the pelvis (five patients), the average length of the tumor was 10 cm (range, 4-15 cm). MR imaging confirmed an intramedullary lesion in all patients, with extension into the soft tissues in eight patients and no identifiable soft-tissue mass in the remaining four patients. Four of the five pelvic tumors had a prominent soft-tissue mass, whereas only four of the seven long bone lesions revealed a soft-tissue mass that was, in all instances, small. The tumor was hypointense on T1-weighted images and showed heterogeneous signal intensity on T2-weighted conventional and fast spin-echo sequences. We saw low signal intensity (short T2) in eight patients and homogeneous hyperintense signal intensity in one patient. In the remaining three patients, T2-weighted spin-echo sequences obtained with fat saturation showed high signal intensity (long T2) in the tumors. CONCLUSION: Primary leiomyosarcoma of bone is a rare tumor that on radiography reveals no matrix and on MR imaging reveals areas of T2 shortening in relation to fat on conventional and fast spin-echo sequences.