| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
- NP (7) - PML
-
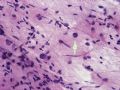
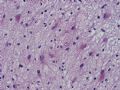
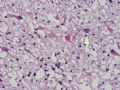
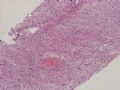
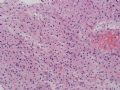
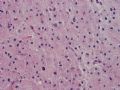
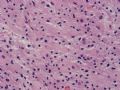
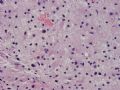
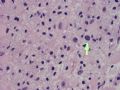
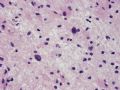
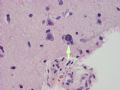
The following photos are taken from a stereotactic brain biopsy from the right frontal lobe of a 22-year-old man with AIDS. He complained of progressive headaches, and brain MRI found many non-enhancing lesions in the subcortical and deep white matter. Figures 1-2 are smear cytology, figures 3-4 are frozen section, and figure 5-12 are from paraffin sections at various magnifications. What are your differential diagnoses?
-
本帖最后由 于 2007-05-01 10:39:00 编辑

聞道有先後,術業有專攻
The smear, frozen section and paraffin sections show reactive astrocytosis, abundant foamy macrophages, and isolated atypical cells with enlarged, hyperchromatic and oval nuclei with abnormal chromatin pattern. These changes are diagnostic of progressive multifocal leokoencephalopathy (PML) caused by reactivated JC virus infection of brain parenchyma, a disease seen predominantly in immunosuppressed hosts (HIV infection, cancer patients with or without chemotherapy, immunosuppressive therapy after organ transplantation).
JC virus is a type of human polyomavirus (used to be papovavirus) related to BK virus and SV40 (simian vacuolating virus 40 or simian virus 40). JC viral infection is very prevalent - an estimated 70~90% of adults have serologic evidence of past JC virus infection, usually in childhood. In immunocompetent hosts, JC virus remain dormant in nuclei of rare scattered glial cells in brain and spinal cord parenchyma. With immunosuppression, the dormant JC virus in these cells may be reactivated and start active replication, causing cell death and tissue destruction. In the genitourinary tract, BK virus acts in a similar way. The name JC is derived from the initials of the name of one of the first patients with PML from which the virus was isolated. It has nothing to do with the CJ in CJD, or Creutzfeldt-Jakob disease
PML lesions are found in white matter and at the corticomedullary junction of cerebral and cerebellar cortex. They are variable in size. The typical white matter lesions show loss of myelin and oligodendrocytes, scattered reactive astrocytes, and varying numbers of foamy macrophages. Inflammatory infiltrates are scant is any. The pathognomonic finding is two types of virally infected glia - (1) infected oligodendrocytes or type 2 PML cells with oval enlarged showing replacement of granular chromatin by basophilic or amphophilic, homogenized, ground-glass like viral inclusion bodies (different from eosinophilic viral inclusion bodies of Cowdry type), and (2) infected astrocytes or transformed astroctytes or type 1 PML cells with markedly enlarged, oval and MIB-1-positive nuclei showing corsely granular chromatin pattern and no viral inclusion bodies.
PML is a disease with grave prognosis. Although anecdotal cases of spontaneous remission have been reported, most cases diagnosed of PML dies within one year regardless of the cause of immunosuppression. Antiviral therapy has little beneficial effects.
Important differential diagnoses of PML include (1) varicella-zoster encephalomyelitis (demyelinating, often hemorrhagic and necrotic lesions with glial cells showing eosinophilic intranuclear viral inclusions), (2) acute demyelination (multiple sclerosis), (3) white matter damage by chemotherapeutic agents (such as methotrexate and cyclophosphamide), (4) toxoplasmosis (often suppurative, necrotic and hemorrhagic), and (5) treated CNS lymphoma. Finding the pathognomonic type 1 and type 2 PML cells is the key.

聞道有先後,術業有專攻