| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
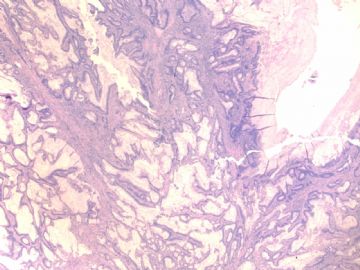
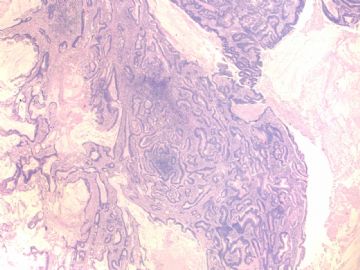
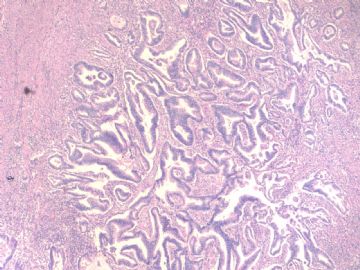
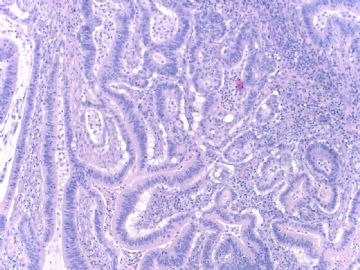
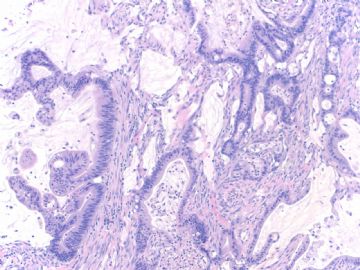
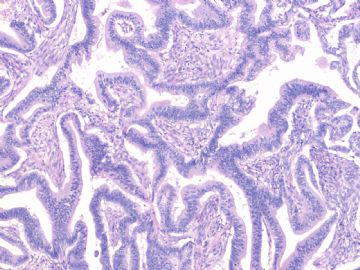
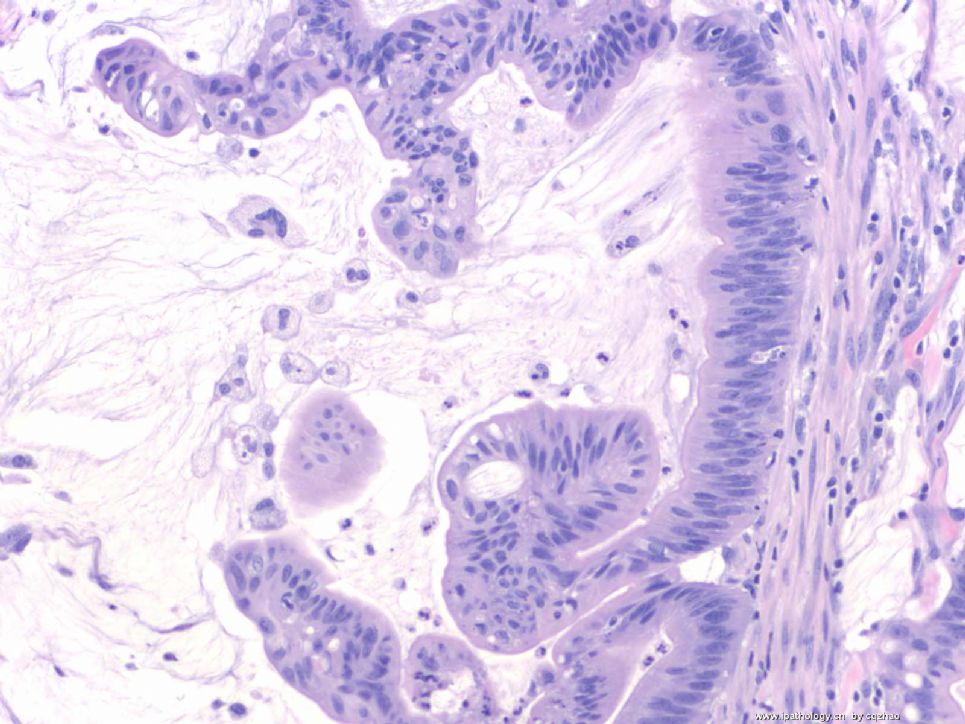
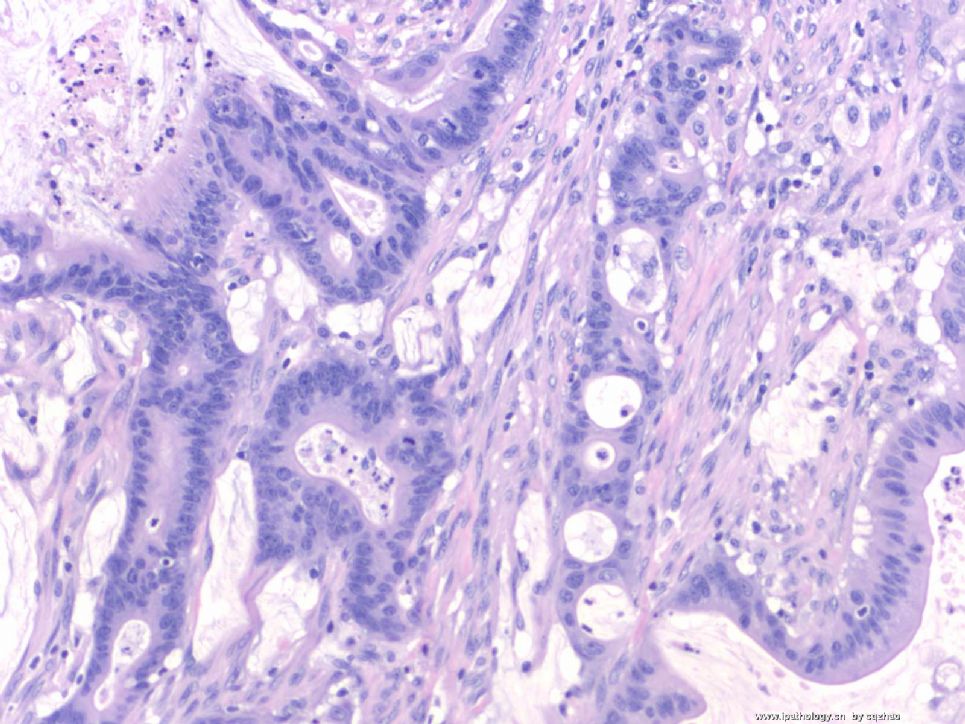
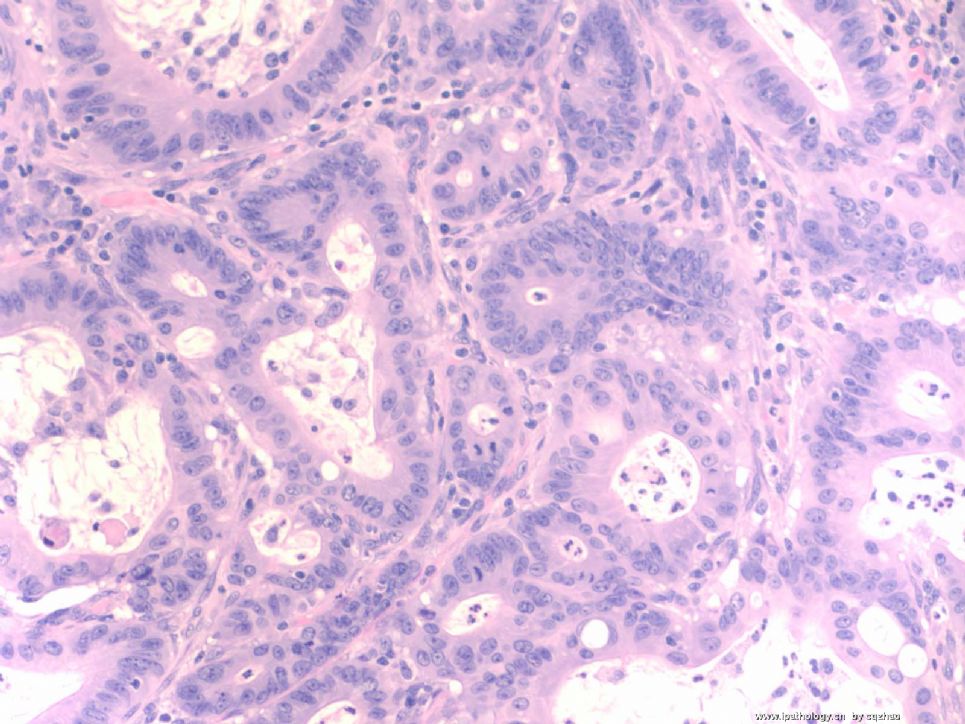
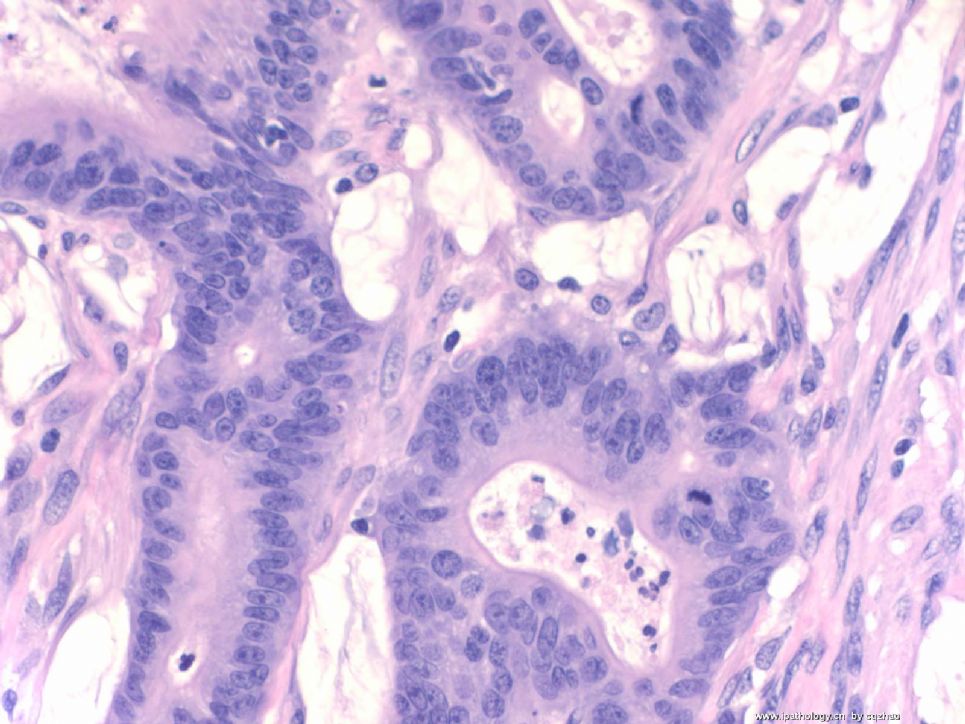
- B1529大肠腺癌转移子宫内膜 in 60 y women without history (cqz 5)
60 y/f had hysterectomy for endometrial lesion. Intraoperation evaluation: 4x3 cm endometrial tumor with 30% of myometrial invasion.
Now you have perminant H@E slides.
Key:
F1-2: 20x
F3: 40x
F4-6: 100x
-
本帖最后由 于 2009-03-22 12:15:00 编辑
相关帖子
No history.
morphologic features caused to do the IHC.
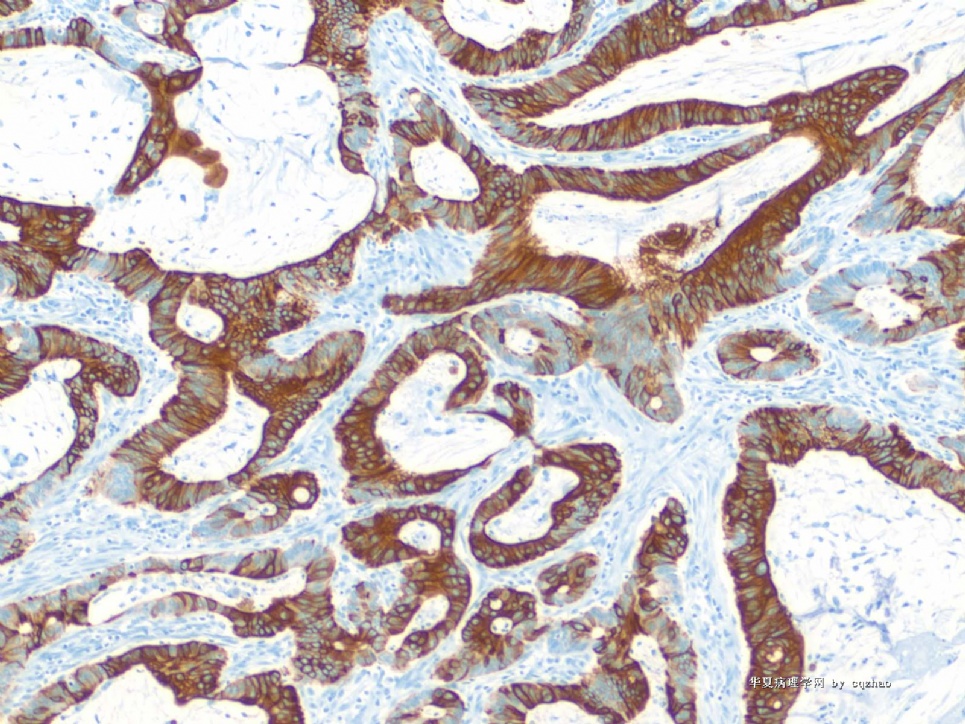
Diagnosis of metastatic GI ca was based on the morphology and more based on the IHC.
In fact the diagnosis: adenocarcinoma.
Comment: mostly from GI metastasis. Strongly suggest to check GI primary.
No more report in our system. This is a outside patient. Do not know if primary ca is found in colon.
-
本帖最后由 于 2009-03-16 02:22:00 编辑
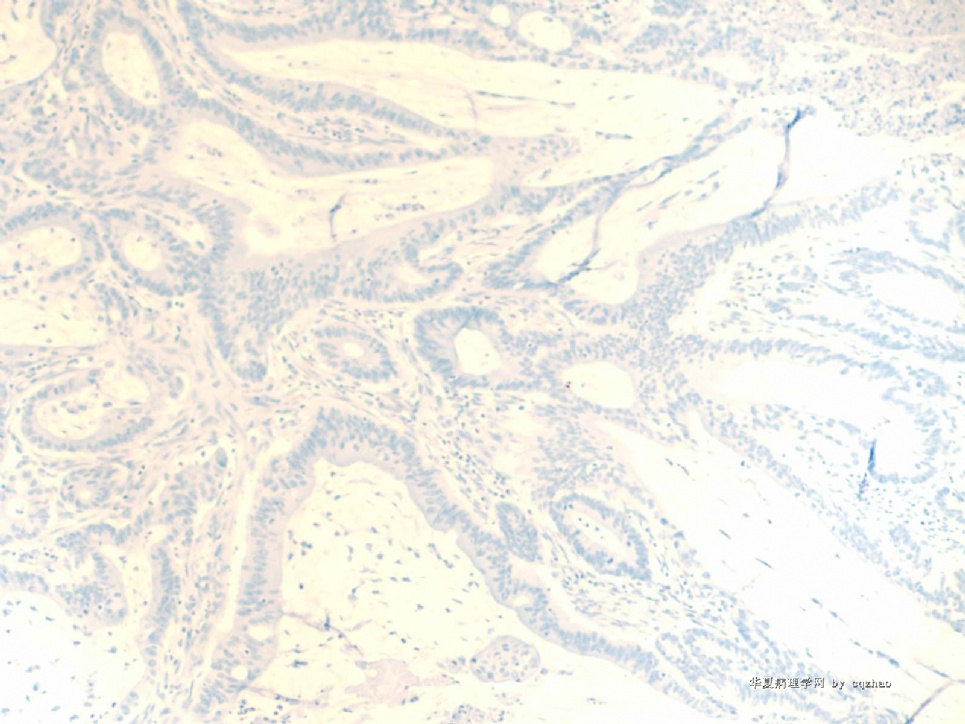
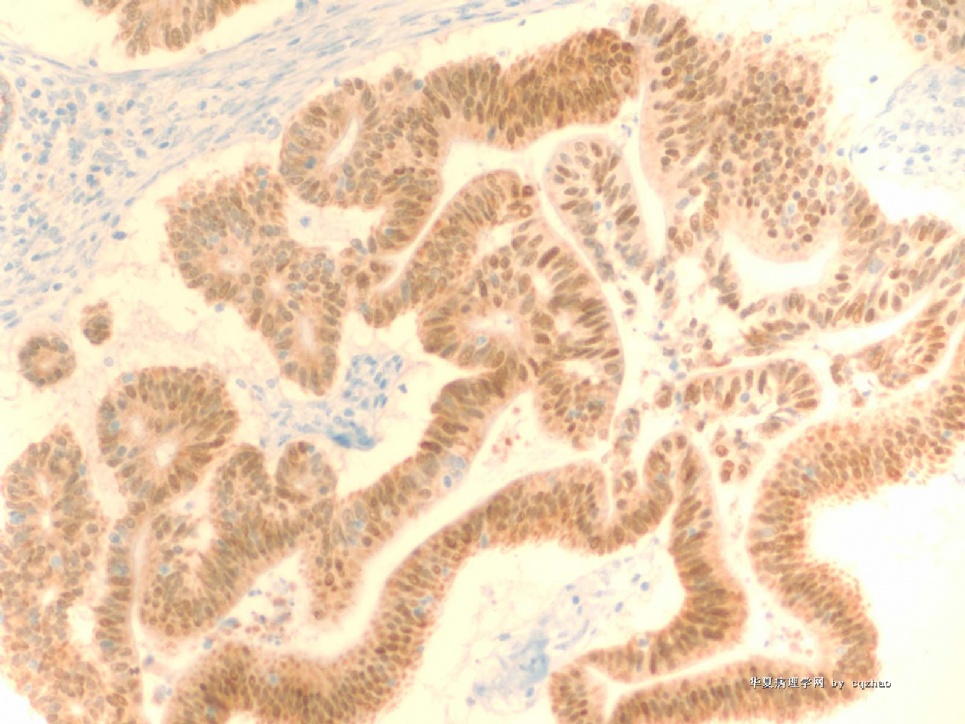
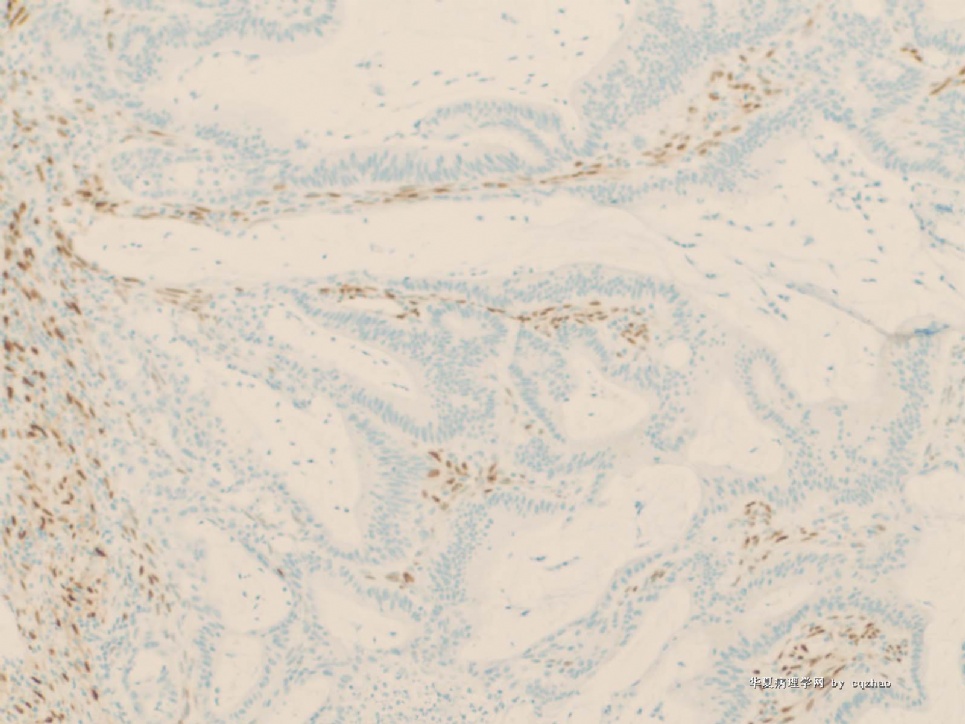
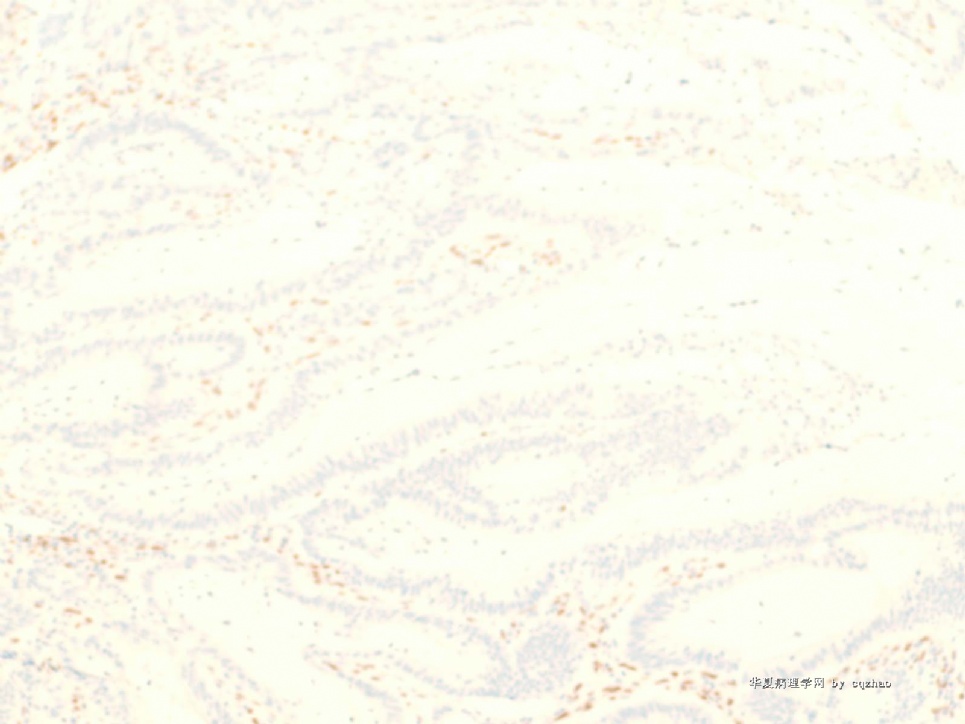
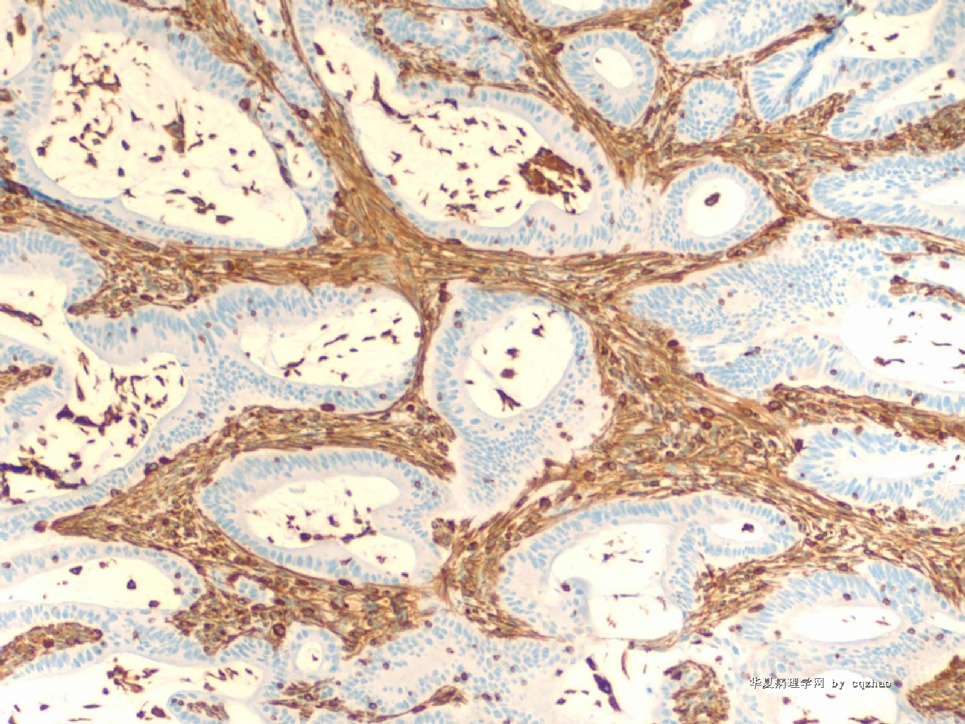
The pathologist did some IHC on endometrial biopsy specimen (biopsy performed in other hospital) and found some surprise pattern. The stains were performed on the hysterectomy specimen also. IHC result seen below.
Key:
f1. CK7
f2. CK20
f3. CDX2
f4. ER
f5. PR
f6. Vimentin
名称:图1
描述:图1
名称:图2
描述:图2
名称:图3
描述:图3
名称:图4
描述:图4
名称:图5
描述:图5
名称:图6
描述:图6
-
More recent history: The patient was present with vaginal bleeding. Endonetrial biopsy was performed in outside hospital and diagnosed as endometrial carcinoma, nuclear grade 2. The women came to our hospital to see gynecologist. The slides of outhospital were sent to our hospital for evaluation. The patient had hysterectomy before our pathologist signed out the case.
-
本帖最后由 于 2009-03-08 10:33:00 编辑
-
Atypical polypoid adenomyofibromas (atypical polypoid adenomyomas) of the uterus. A clinicopathologic study of 55 cases.
Division of Surgical Pathology, Stanford University Medical Center, CA 94305, USA.
We present the clinicopathological and immunohistochemical features of 55 atypical polypoid adenomyofibromas, a definitional expansion of an entity previously reported as "atypical polypoid adenomyoma" (APA) of the uterus. Patients ranged in age from 25 to 73 (mean, 39.9) years. All but two of the patients were premenopausal, and 14 were undergoing evaluation for infertility. Histologically, the lesions featured a biphasic proliferation of architecturally complex and cytologically atypical endometrial glands within a myofibromatous stroma. The histologic pattern ranged from widely separated and loosely clustered irregular but branched glands embedded in broad zones of cellular myofibromatous stroma to those possessing crowded, markedly complex, branching glands separated by sparse intersecting fascicles of fibromuscular tissue. The stroma in all cases was actin or desmin positive or both. Morular/squamous metaplasia was present in all but two cases and florid in most. All cases exhibited architecturally complex glands, and in 25 cases the architectural complexity was indistinguishable from that of well-differentiated endometrial adenocarcinoma, as we have defined it; that is, they had a high architectural index. Twenty-nine patients were initially treated with polypectomy or curettage followed by hormonal therapy; persistent or recurrent APA developed in 45% of the patients in this group (33% with low architectural index vs. 60% with high architectural index). Five patients had successful pregnancies despite persistent disease. Superficial myoinvasion was identified in the hysterectomy specimen in two of 12 APAs with a high architectural index but not in 21 APAs with a low architectural index. All patients are alive and well 1 to 112 months after diagnosis (mean, 25.2 months). On the basis of this study, we propose that APAs with markedly complex glands (high architectural index) be designated "atypical polypoid adenomyofibromas of low malignant potential" (APA-LMP) to emphasize the potential risk for myometrial invasion. A treatment program featuring local excision accompanied by close follow-up is warranted for APA despite the presence of recurrent or persistent disease. Patients with APA-LMP may also, in selected cases, be managed with less than hysterectomy, although (as with the usual well-differentiated carcinoma) there is a small but definite risk associated with this approach
A good paper about APA from Stanford more than 10 years ago
Am J Surg Pathol. 1996 Jan;20(1):1-20.