| 图片: | |
|---|---|
| 名称: | |
| 描述: | |
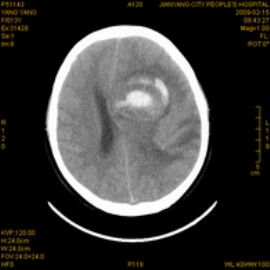
- 左颞顶额叶肿瘤(090843)
-
本帖最后由 于 2009-02-23 01:27:00 编辑
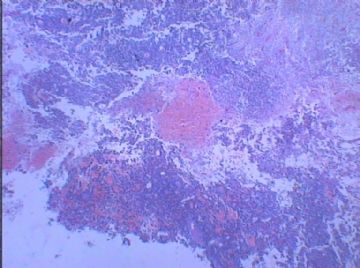
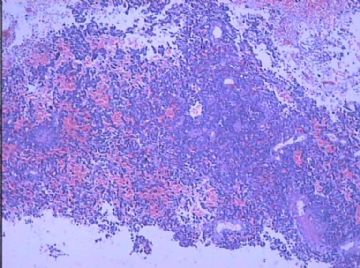
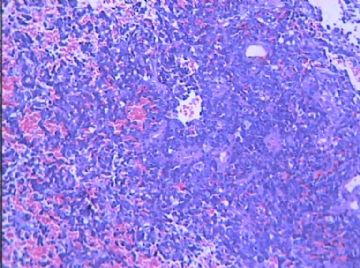
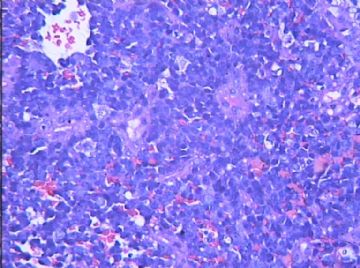
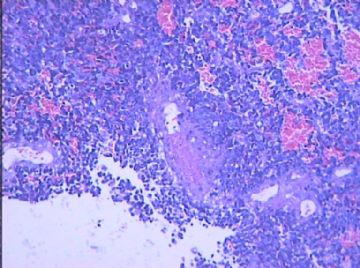
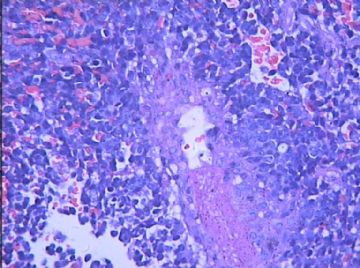
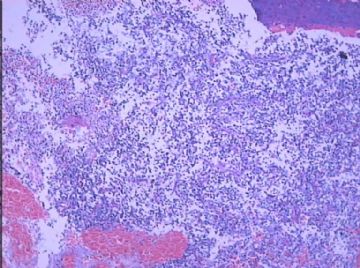
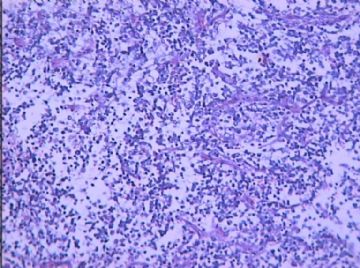
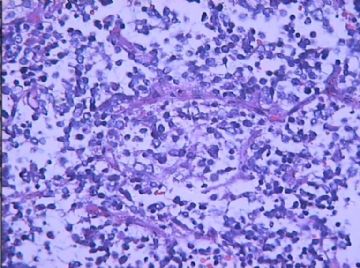
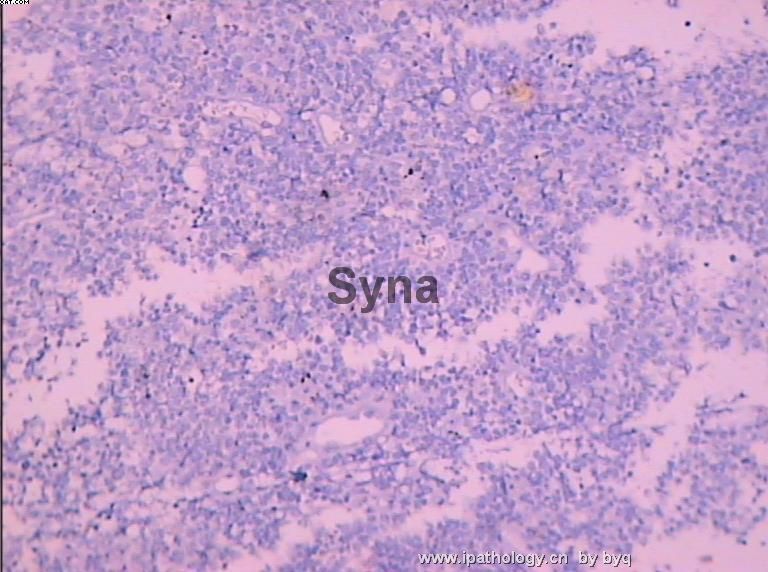
There are hypercellularity, focal tumor necrosis, and marked nuclear atypia consistent with a malignant neoplasm. The differential diagnoses for this "small blue cell malignancy" found in the cerebrum of a 13 year old child include (1) supratentorial primitive neuroectodernal tumor (PNET), (2) atypical teratoid/rhabdoid tumor (AT/RT), (3) small cell variant of glioblastoma, (4) lymphom, and (5) anaplastic ependymoma. I do not see any feature (perivascular pseudorosettes, ependymal canals, perinuclear halos) suggestive of ependymal differentiation, so (5) is unlikely. LCA is reportedly negative, so (4) is unlikely. GFAP is reportedly positive, but I would like to see the extent (% of cells) and intensity of positive staining. PNET may have some cells that are GFAP-positive, while small cell glioblastoma may show only few GFAP-positive cells. To further characterize the malignancy, I suggest the following immunohistochemical stains - synaptophysin, NSE, EMA, and smooth muscle actin. I will wait for these results before making a final diagnosis.

聞道有先後,術業有專攻
| 以下是引用mjma在2009-2-23 1:26:00的发言: There are hypercellularity, focal tumor necrosis, and marked nuclear atypia consistent with a malignant neoplasm. The differential diagnoses for this "small blue cell malignancy" found in the cerebrum of a 13 year old child include (1) supratentorial primitive neuroectodernal tumor (PNET), (2) atypical teratoid/rhabdoid tumor (AT/RT), (3) small cell variant of glioblastoma, (4) lymphom, and (5) anaplastic ependymoma. I do not see any feature (perivascular pseudorosettes, ependymal canals, perinuclear halos) suggestive of ependymal differentiation, so (5) is unlikely. LCA is reportedly negative, so (4) is unlikely. GFAP is reportedly positive, but I would like to see the extent (% of cells) and intensity of positive staining. PNET may have some cells that are GFAP-positive, while small cell glioblastoma may show only few GFAP-positive cells. To further characterize the malignancy, I suggest the following immunohistochemical stains - synaptophysin, NSE, EMA, and smooth muscle actin. I will wait for these results before making a final diagnosis. |
-
本帖最后由 于 2009-02-25 11:13:00 编辑
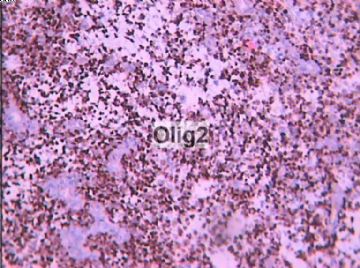
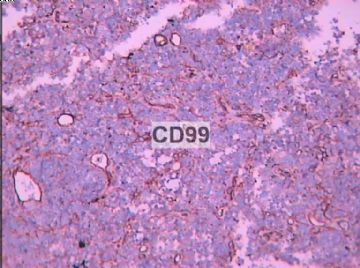
The high MIB-1 labeling index is consistent with a malignant neoplasm - not a surprise. I am not very familiar with the practical use of CD99 and olig2. NSE and synaptophysin both appear negative, making PNET unlikely. SMA appears negative, making AT/RT unlikely. GFAP appears positive and EMA appears negative, but I would like to see high-power (400x) view of these to make sure GFAP immunoreactivity is not background staining and no paranuclear, dot-like EMA immunoreactivity is seen. If GFAP is truly positive and EMA truly negative, this would fit the diagnosis of WHO grade IV glioblastoma of the small cell variant.

聞道有先後,術業有專攻
-
I have little experience with olig2 stain, so cannot comment on the significance of its positive staining in this case. I do not see features characteristic of oligodendroglioma, so would still favor WHO grade IV glioblastoma, small cell variant. The most difficult differential diagnosis in this young patient would be PNET, but negative staining of NSE and synaptophysin pretty much rule it out.

聞道有先後,術業有專攻
| The high MIB-1 labeling index is consistent with a malignant neoplasm - not a surprise. I am not very familiar with the practical use of CD99 and olig2. NSE and synaptophysin both appear negative, making PNET unlikely. SMA appears negative, making AT/RT unlikely. GFAP appears positive and EMA appears negative, but I would like to see high-power (400x) view of these to make sure GFAP immunoreactivity is not background staining and no paranuclear, dot-like EMA immunoreactivity is seen. If GFAP is truly positive and EMA truly negative, this would fit the diagnosis of WHO grade IV glioblastoma of the small cell variant. |
-
zhang197510 离线
- 帖子:409
- 粉蓝豆:2973
- 经验:448
- 注册时间:2009-03-22
- 加关注 | 发消息
-
liangjinjun 离线
- 帖子:2328
- 粉蓝豆:2
- 经验:2457
- 注册时间:2007-08-07
- 加关注 | 发消息